My provider reset my APAP to a range of 10cm - 14cm about two weeks ago.
Ever since, my AHI has been trending upwards. When I wake up to go to bathrm, I notice that the air pressure is running at 11cm.
Prior to this APAP reset, I had set my machine at a fixed 14 cm, and was observing my AHI consistently trending downwards.
I don't want to wait two months for another provider appointment to get another pressure adjustment.
Any recommendations are greatly appreciated !
My thoughts are that if your apnea is all obstructive, the APAP can adjust pressure quite effectively in most cases. However, most often a narrow pressure range is more effective than a wide range. Bringing the minimum pressure up tends to have more effect than increasing the maximum pressure. If there is significant central apnea, one may be able to do better with a fixed pressure.
This said, a picture is worth about 1000 posts. If you want to post a SleepyHead screenshot of your Daily Detail report I could be much more specific with comments, and help you out on how to read the report. It would be helpful to post a shot of where you were getting to with the fixed 14 cm and a typical one now with the auto range. If you need any help posting the screen shot, just ask.
The alternative to waiting for another appointment is to make your own pressure adjustments if you are comfortable doing that. Some are, and some are not. If you need help doing that, just ask. Here is a link to the technical manual for your machine. The Provider Menu instructions start on page 4-18. You can read it over and decide if you feel confident making changes. I can make a pressure change on my machine in about 15 seconds. It just depends what you are comfortable with.
Did he reset it during a visit or remotely? 2 choices, insist on a same day appointment or take charge for yourself.
Download and install Sleepyhead if you have not done so. This will provide you with data from which to make good decisions. An extreme improvement if you are using over the air data. If you post your nightly charts with these charts Events, Flow Rate, Pressure (not mask pressure), Leak Rate, and Snore. If you had a ResMed machine the Flow Limit also. I'm sure Sierra would be more than happy to provide thoughts on your charts
Ok, I had my cpap set, fixed at 14 cm and I started seeing AHI pretty close to 5.
After being told by nurse to set apap to 10 - 14 cm I am seeing AHI trending up.
I know how to change the air pressure or the pressure range.
I am pretty aggressive about my health care goals and do not need to follow the health providers guidance if their "bar is set too low" for success.
thanks for any insights ! dmypub
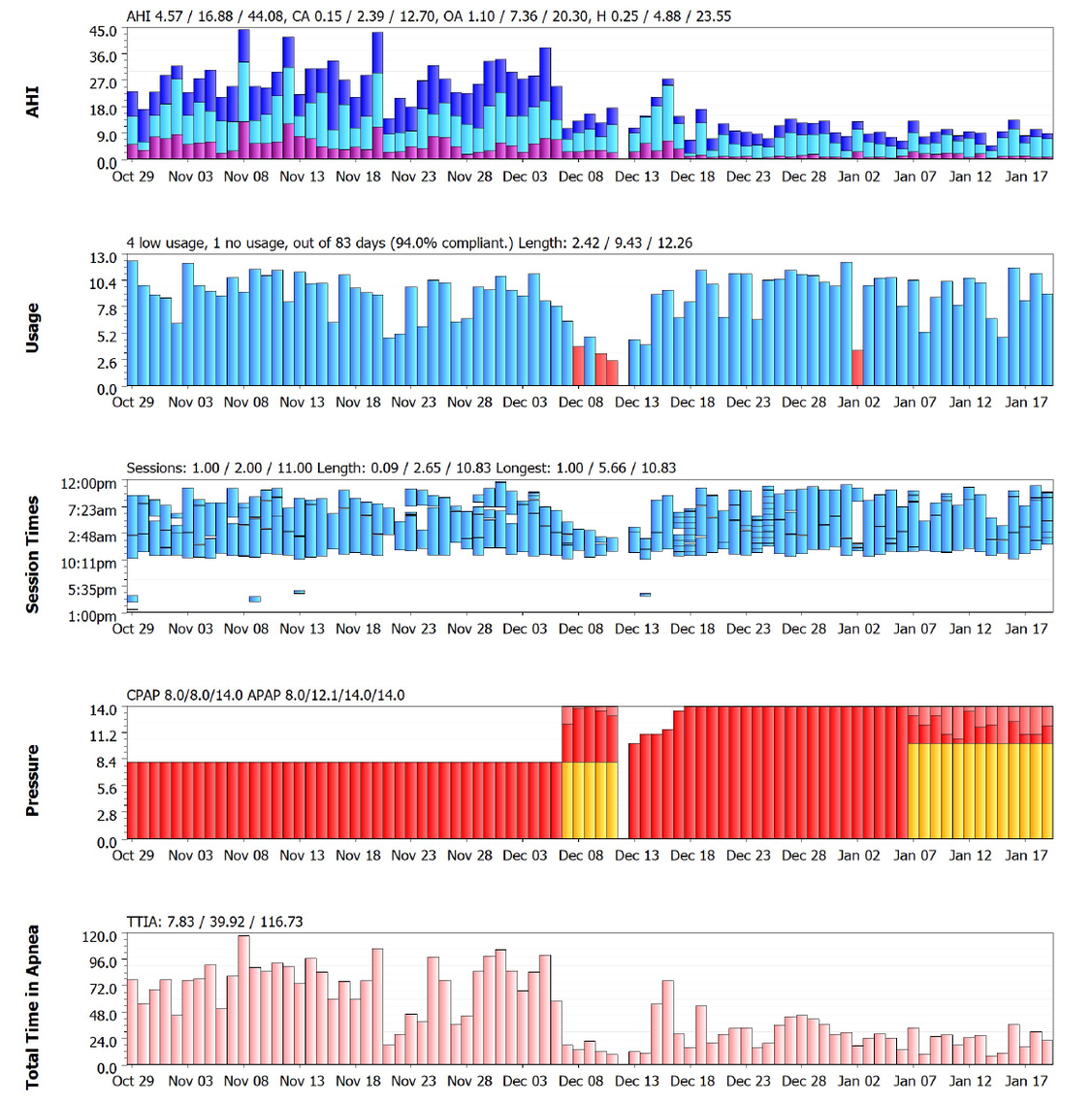
What I see is:
You can get a more accurate read of the average AHI for each mode from the SleepyHead Statistics page. Each time you change the treatment settings it should start a new line, with the start and end date, the average AHI, and what the settings were. That would let you compare the modes tried to date more accurately. A duration of one night at a certain setting is fairly meaningless though. I think a minimum of 7 days is required to give the mode a fair evaluation, and a month is better still.
If you can post a daily Detail page it would be much more helpful. January 7th would be a good night to post. Are you using the Flex setting on the machine? If so, one possible quick improvement could be to turn it off or set it to zero.
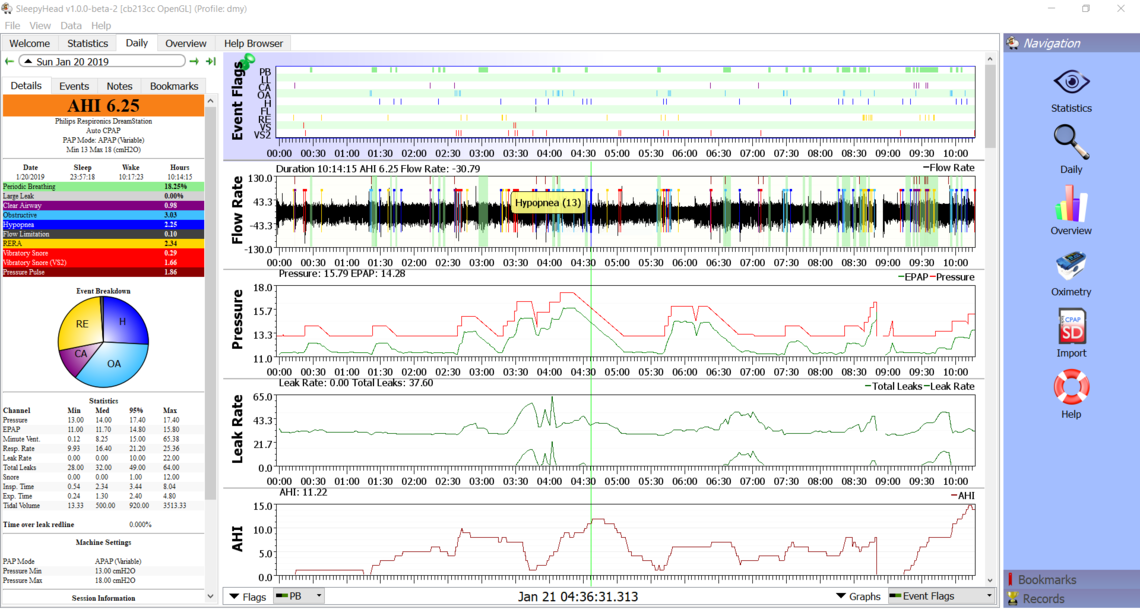
The changes you made to max and min pressure have helped. The next thing I would do is turn off the Flex. If you look at the Pressure chart, the red line shows pressure on inhale (IPAP). The green line is kind of the pressure on exhale (EPAP). As you move your cursor across the screen, the numbers above the pressure graph will show the pressure at that specific time. So, if you match the cursor up with an event you can see at what pressure it occurs at. The issue with leaving Flex turned on is that events can occur on exhale as well as inhale. The lower pressure can create events. My experience is that it is best to turn Flex off on a DreamStation. This may reduce your event frequency, and possibly your pressure too.
The other point of significance in this chart and the other one from Jan 7, are the green highlighted areas which Respironics calls periodic breathing. ResMed flags something similar as Cheyne Stokes Respiration (CSR). This is what CSR looks like on a close up breath by breath basis.
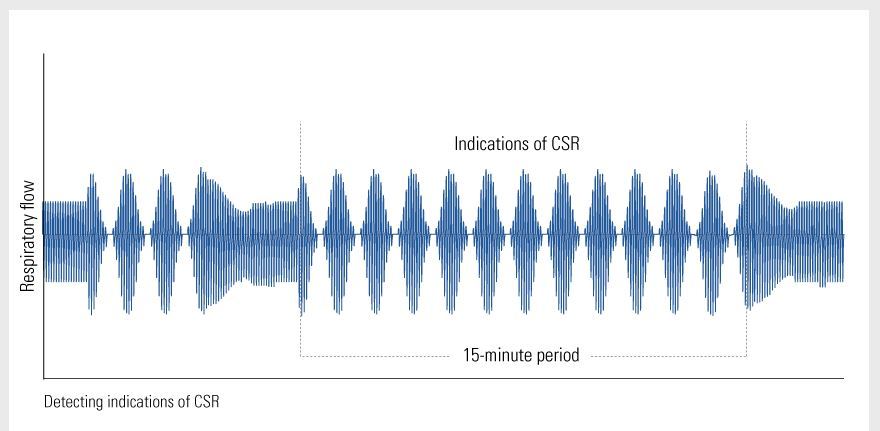
What you should do is put your cursor over one of those areas where there is green highlighting and CA events flagged. Then left click repeatedly or use the up arrow to expand the scale to see the breath by breath detail. If looks like the CSR image above this is something to discuss with your GP, and/or cardiologist. It could be heart issues, or heart medication, other medication, etc. You do not happen to live at a higher elevation? That can aggravate it too. If you can post a zoomed in screen of the periodic breathing area including the central events, I can give you my thoughts on how it compares to what I am seeing in my own charts.
I have seen a very small amount of CSR flagged in my charts, but over time I see a very small amount. The last time I saw it was over two months ago. With a ResMed the CPAP stats page in SleepyHead includes the % of CSR.
As far as your settings go the only change I would make now would be to turn Flex off. Future opportunities may be to lower the max pressure below 18 cm, but I wouldn't jump into that until you see what setting flex to zero or shutting it off does.
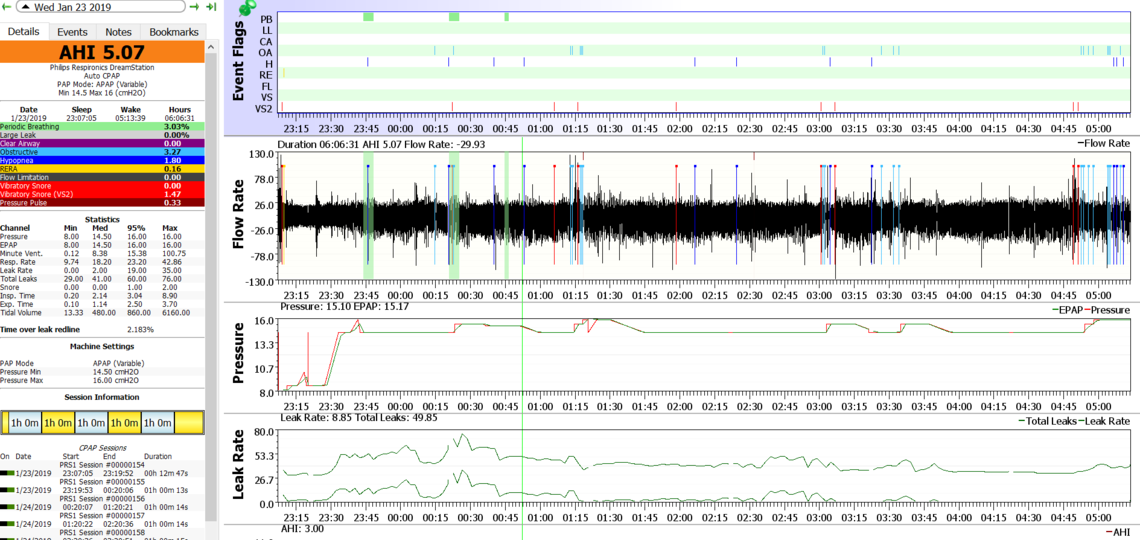
January 7th
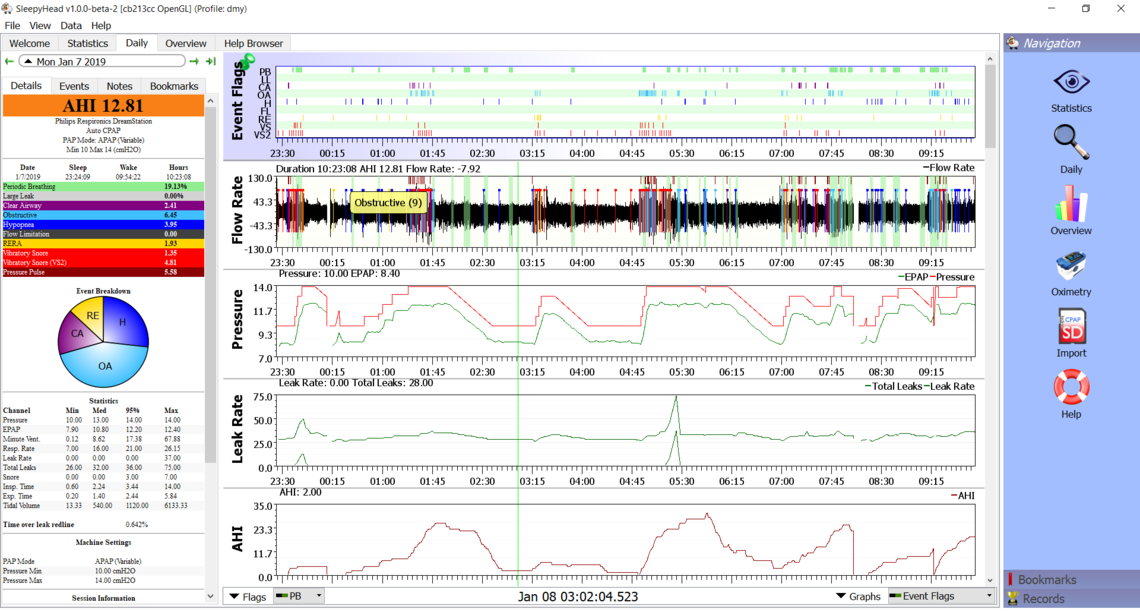
What this chart shows is that your 95% pressure is equal to your maximum pressure of 14 cm. You are also getting many of your events, mainly obstructive, but a significant number of CA events too at maximum pressure. In short it is showing you would benefit from a higher maximum pressure. I have never found the AHI graph because of the way it records to be really helpful. The Event flags show just as well where the events are occurring. Instead of the AHI graph you may want to bring up the Minute Ventilation graph if DreamStation provides that data. I am finding it useful in identifying areas of interest with my own central apnea issues.
I would suggest cleaning up the format so more information can show in more detail. Use File, Preferences, Appearances, to uncheck the box that says "Show AHI breakdown Pie Chart", or something like that. It is kind of redundant. Same with the Navigation tool bar on the right. It just takes up space. F10 to toggle it off on a PC. F8 or Shift F8 to toggle it off on a Mac I believe. And if you use the Orange "Write a reply" button at the bottom of the thread you get a full width window to post an image in.
Sorry to question Sierra but did you mean maximum of minimum?
"In short it is showing you would benefit from a higher maximum pressure."
No problem, I often do the dyslexic thing. However in this case did mean a higher maximum pressure. The machine was bumping into the max of 14 cm, and events were still occurring at 14 cm. This is most often a sign the pressure max is too low. The OP has done that and increased the max to 18, and got an improvement. The remaining issue is that AHI is still a bit high with a pressure of 18 cm, and the machine is not even trying to go higher. I would hope things improve by shutting off Flex. The next step may be to reduce the maximum some to see if there is a "happy spot" in there somewhere that will minimize OA events while limiting CA events. The other tool still left in the toolbox is the cervical collar trick suggested by bonjour in another thread.
Success in another forum similar chart
http://www.apneaboard.com/wiki/index.php?title=Optimizing_therapy#Positional_Apnea
Auto CPAPs work fine for most people but certainly not for all. There are a few things which can prevent them from doing their job properly.
I wonder why the nurse suggested that you change from 14 to 10 - 14. The minimum pressure isn't that low, so you won't get much improvement in comfort. And if you were happy enough at fixed pressure, why muck around with it? If they wanted you to go on auto mode, why not a slightly higher max pressure to see if that reduced your AHI further? Setting the max pressure at the same levels as your fixed pressure is not going to reduce obstruction at all.
Going with that range over the fixed pressure could reduce Central events when not at max pressure. I do not know this users history so this is a generalization. BTW, that technique does not always work or it will only seem to work because Central elements on a CPAP are usually consistently inconsistent.
Fred
I have actually found benefit in raising the minimum pressure while leaving the maximum pressure fixed. I only like to raise maximum pressure as a last resort. Raising minimum pressure often eliminates the trigger events which the auto machine needs to be prompted to raise the pressure.
However in this case, with a fixed 14 cm not achieving <5 AHI kind of indicates max pressure will have to be increased at some point. If Flex is being used, I would discontinue that first though.
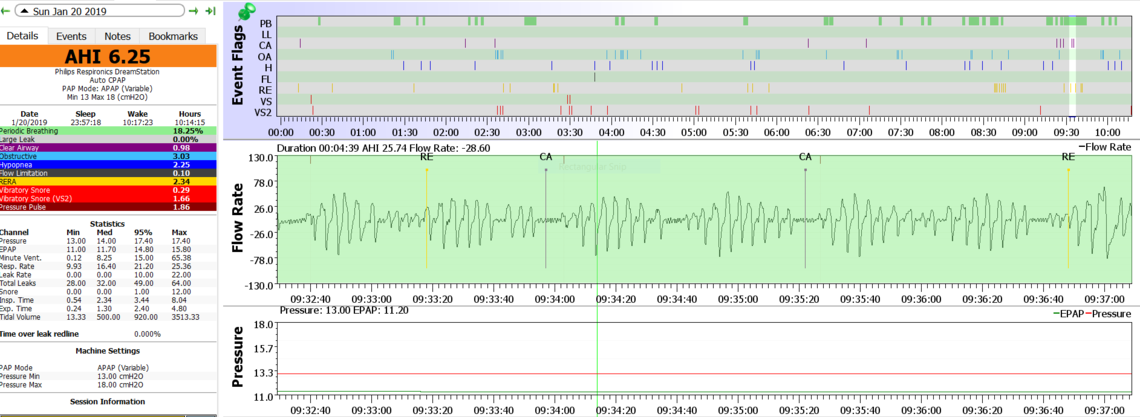
Periodic Breathing Close Up. I live at 5000 feet altitude. I take blood pressure meds. I also regularly have atrial fibrilation issues. I turned off my flex for tonight. Thank you for your help. Not getting this kind of analysis from my provider !
Yes, in my non medical professional opinion, that looks to me like Cheyne-Stokes Respiration. I have experienced events that look quite similar. Certainly the 5000 foot elevation is not helping. I was taking a minimal dose of a beta blocker, bisoprolol, and I convinced my GP doctor to cut the dose in half. I think he was a bit skeptical about it, but said my blood pressure was fine with the lower dose, and went along with it. With central apnea it is hard to attribute cause and effect, but I think it has reduced my frequency of CSR. Beta blockers not only reduce blood pressure but they mainly do it by reducing the pulse rate. I think in turn that reduces blood flow which can aggravate central apnea. The literature reports an association of CRS with atrial fibrillation to.
There is a good blog here by an MD, Robert Thomas, on Complex Sleep Apnea that you may be interested in reading. He mentions that there is some indication a drug intended to treat elevation sickness, acetazolamide, can reduce central sleep apnea. Perhaps something to have a discussion with your doctor about. I believe it is basically a diuretic which is considered a safe drug to treat blood pressure long term.
You may find this study abstract of interest:
thank you for these references. I will study these and discuss with Dr. Here's what I looked like last night with FLEX OFF. I feel like I got pushed pretty hard - little bit sore today, but one of the best AHI readings I've achieved. STILL fighting to get a mask that doesn't wake me up with "mask farts" and leaking whistles.. Supposed to be getting resmed F30 next week to test. thanks again !
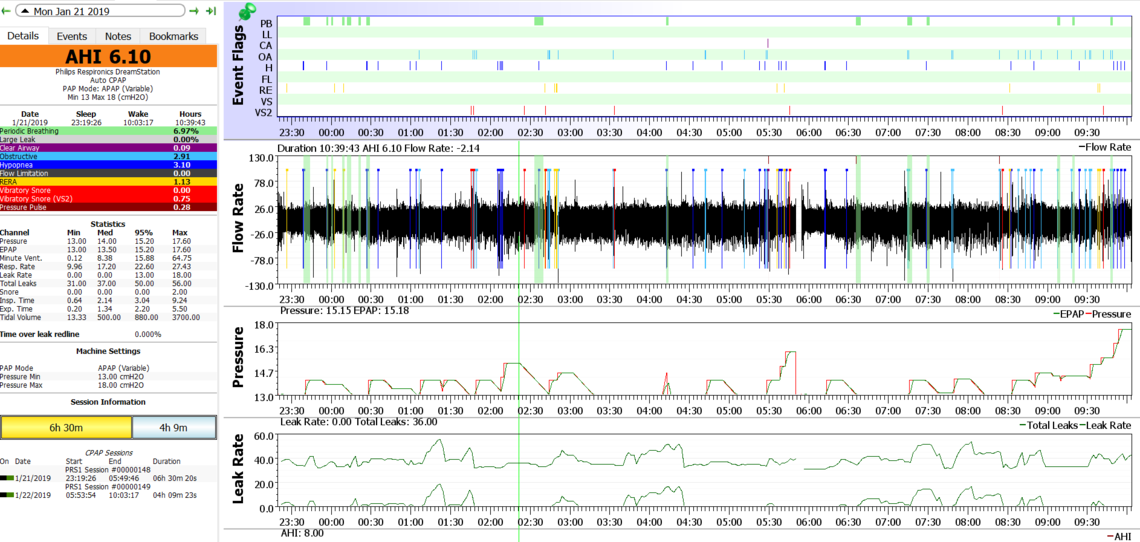
I think what I would try next is a tighter range. You are still getting quite a few events where the machine seems to be getting caught with not enough pressure. At the maximum pressure end it is not even going up to full pressure, and you would not lose much by restricting the max pressure. It is always a bit of a guess, but I think I would try 14.5 min and 16 max. Your minimum pressure is getting up there, so you may want to use the DreamStation SmartRamp feature. You should be able to select it and then choose a ramp start pressure. I would suggest a ramp start of 7-8 cm, whatever feels comfortable to you. It should hold the pressure at that value until it detects you are sleeping, thus making it easier to go to sleep. When you go to sleep it should then ramp up to your minimum treatment pressure.
On the mask farts issue, some people report getting a better seal and better comfort by using a layer of old cotton T-shirt material as a liner. You would have to cut it out in the shape of your mask seal plus a bit extra. Remzzzs is one commercial brand. I have no personal experience though.
dmypub look at 3 min segments (2-5 min segments will show details of the pattern and make it distinguishable) of several of the CSR/periodic breathing and print them for your doctor. On multiple days too, If you have Sleepyhead on a laptop take it in with you so your doctor can personally evaluate several of these segments. Print any 10 min segments of CSR too.
It's the evenness of the increase in breathing with the decrease of breathing with a Central Apnea in the middle that defines this pattern.
Another similar pattern that is somewhat similar starts with an OA followed by a large recovery breath and each successive breath is smaller then you have another OA event and repeat.
Cheyne-Stokes Respiration (CSR): CSR is a breathing pattern characterized by cycles of crescendo-decrescendo changes in tidal volume followed by central sleep apneas. A complete cycle of apnea, hypopnea, hyperpnea, and hypopnea leading to the next apnea usually takes about 45 seconds but may be longer. At least ten consecutive minutes of these cycles should be recorded before CSR can be diagnosed.
Based on the above look for a CSR series that is 10 min plus and print that for your doctor as that appears to be a diagnostic standard. BTW CSR is fairly common in individuals with CHF. 25-40% of CHF patients have CSR
To have these CSR events once in a blue moon I would just dismiss them, but regularly and I would have them professionally checked out.
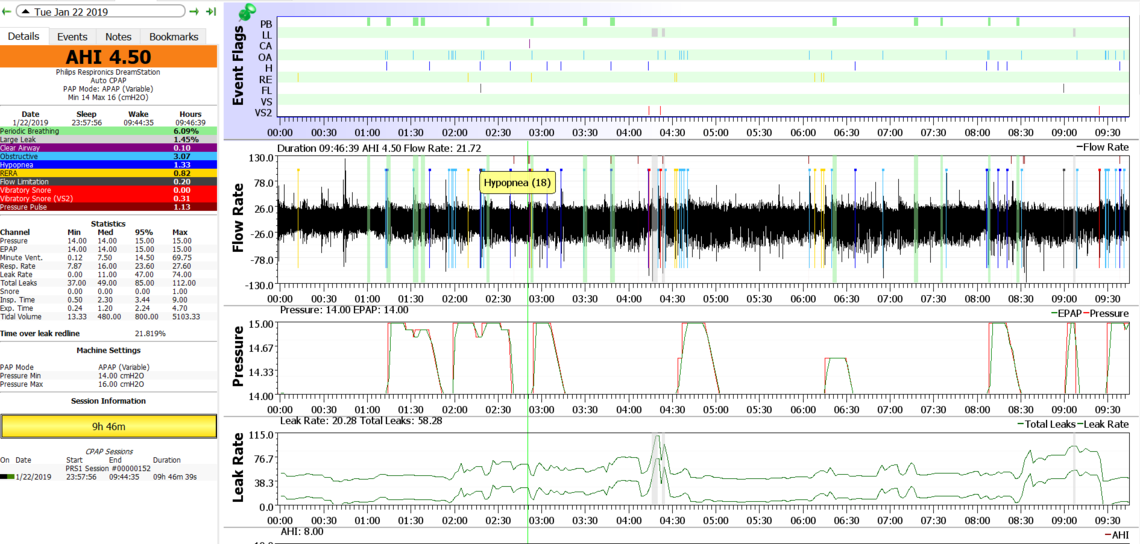
Thank you so much for your guidance. Last night was the best on record, judging just from the AHI !
I'm curious, if my CSR pattern is an issue why the registered nurse who reviewed my data did not bring it up with me ? Perhaps she looked at my heart history and concluded it was to be expected ? OR, maybe I should seek a different nurse of Dr ?
Thank you so much for your suggestion of using an old T-shirt to muffle the air leak noises - it's been a huge struggle that wakes me up. Slept great last night NOT having to manage mask flapping !
That looks better. Your CA event frequency is very low and the residual is mainly OA and H. The machine did not attempt to go over 15 cm even though you had the max at 16 cm. What seems to be happening is that the machine algorithm is getting caught with the pressure too low, events happen, and it jumps up, and then fairly quickly the machine wants to reduce pressure. The set minimum of 14 cm is likely preventing it from going even lower and making things worse. Unfortunately this quick spiking up and down is a characteristic of the Respironics algorithm. My first thought would be bump the minimum pressure up to 14.5 and try that. If that helps, but there is still high OA, then the next step may be to go to a fixed 15 cm. I wouldn't jump into that yet, as you want to see where the machine wants to take pressure in limited auto control.
On the CSR I would not get too hung up on whether it is or it isn't. I think there is enough there to say there is an issue that should be raised with your GP doctor or cardiologist. Remember that Respironics does not say it is CSR, they just report periodic breathing probably on a basis that may be unique to Respironics. ResMed does report CSR, but again they are probably not all that transparent as to how they do it. This periodic breathing issue may have been there before you went on PAP treatment, and now the only difference is that you have a PAP machine reporting it to you, compliments of SleepyHead. Or, it may not have been there before, and the PAP treatment in the pressure range you have of about 15 cm is causing it, or aggravating it. That is of bigger concern, and again I would recommend discussion with the appropriate medical professional, like a cardiologist.
If they feel it is something that should be addressed, then that drug (Acetazolamide) I mentioned before may be of some help. Another approach that is used is to switch machines from the standard APAP you are using now to an ASV machine. There are risks associated with that too, and while it probably will reduce CSR and central apnea, it may or may not improve outcomes. That is something to be discussed fully with your health care professionals. Here is another reference you may find of interest.
This all said I would think that your elevation of 5000 feet is a factor in this, and it may not be fair to assume this is a heart issue. There can be other causes, and that drug for elevation sickness may have some benefits. And, I also think with a few more tweaks you may be able to get your AHI under the treatment guideline of 5.
Keep posting. I think you are making good progress.
I bumped the pressure to 14.5 . But had the worst night since starting cpap. Mask kept leaking, even with fabric layer under mask. Finally gave up, exasperated, at about 5 am. Woke up with a serious hangover - like I drank two bottles of wine. Serious eye bags - needing ice. Still recuperating after an hour being up. Does this type of "hangover" make sense due to CPAP ? Thanks.
Well the good news in this one is that your Periodic Breathing seems to be down, and there were zero central apnea events even though the pressure was higher. If you were disturbed with leaks all night that is probably the reason for feeling bad. Simply not enough sleep is the most likely problem.
I see from an earlier post you have a new mask (F30) on order. What mask are you using now? I don't have a lot of experience with full face masks but others here may. Perhaps they may have some suggestions on how to address leaks. From what I can see your mask leaks were much better later in the night, so perhaps you were making progress.
Probably about half of the obstructive events were happening at the 14.5 cm minimum. The next step would be to try a 15 cm minimum while leaving the max at 16. Probably going to make it harder from the leaks perspective though, so sooner or later you will have to solve that one. Perhaps the new mask will be better...
The other issue is that the obstructive events (not so much with the hypopnea) look like they are occurring in clusters. Bonjour has mentioned in another thread that sometimes it is a head positional issue that can be reduced by using a soft cervical collar. They are not too expensive, so at some point that may be worth a try.
I am using a Simplus mask - much less leaking than the respironics amara I started out with. I had minimal leaks at 14 cm with a "t-shirt" fabric under the mask. As long as I can remember, I flip and flop all night long changing position, so maybe I'm putting my neck in some weird position.
I'm taking it easy tonight - my eyes are still puffy. Thanks Canada !
Unfortunately I have no experience with the Simplus mask, but perhaps others do. I have a recollection it is one of the older ones that are supposed to be capable of higher pressures. The Amara I recall got good reviews too. Mask are very individual, and the full face one seem to need lots of tweaking to make them work. I find it amazing that some people on a BiPAP uses these things right up to 25 cm of pressure...
At some point it would make some sense to stop and leave the pressure alone for a while. That could be at 14.5 to 16, or 15 to 16. The machine changes pressure instantly. The user does not adapt to it quite so quickly. The unfortunate part is that obstructive apnea is still showing up with pressures as high as 16. That indicates more pressure is needed. With no central apnea that is a good sign that it is not going to be a problem.
Hope that helps,