Hey folks,
New to the forum and have been enjoying reading some of the opinions and threads on here. I recently did a home test for sleep apnea (using a Philips machine and can't remember the model exactly) and it came up positive for OSA. It showed I had mild OSA with an AHI of 8 with no central apneas. I now need to take these results to my GP to get referred to a sleep clinic etc. With an already low AHI, can I expect much quality of life improvements from getting this treated? My daytime sleepiness isn't too bad, but I do find it almost impossible to stay awake in moving cars etc and do have periods of low mood, which may well be related.
Any opinions much appreciated.
Welcome to the forum. I was diagnosed with a home sleep study as well. The machine I used was a Phillips Alice NightOne. You probably had the same. I went straight from the home study to an APAP machine, but my diagnosis was much higher at 37.
Treating a low AHI is always a dilemma. I can't say there is no discomfort to wearing a mask and using a machine. Some don't find it no problem at all, and others it bothers more. At least initially it is likely to disturb your sleep some. With a low AHI the pressure is also most likely to be lower, and that tends to make for more comfort. On the benefits side, it is much harder to predict. Reducing AHI from 8 to say 1 may not be that great. However, if there are other underlying issues such as RERA, snoring, and flow limitation events which don't get counted in the AHI the benefits may be higher than the AHI would suggest. I don't believe the Phillips machine reports RERA events, or at least my sleep report did not include them. Snoring should be measured though. An in lab test should measure RERA and they get added to the AHI to form the RDI index, which could be higher.
If you go ahead with the in clinic sleep test, you will know more and be able to make a better decision at that point. If things stay pretty much the same you would have the choice of going with a dental appliance or a PAP machine. The dental appliance is more expensive, but may be covered under your health insurance rather than dental insurance, and could end up less costly. If you go the PAP route, which is likely to have the best outcome in AHI, but not necessarily in comfort, I would resist doing a separate additional titration study and just ask for an automatic PAP machine. With your low AHI a ResMed AirSense 10 AutoSet For Her would be probably the best choice if you can wangle it. It is designed for women but can work for men with a lower AHI and less need for pressure. It is the same cost as the standard machine, and can be set to the standard mode if the For Her mode does not work. It just gives you more options.
Hope that helps some,
Thanks for the detailed reply! Yes, the study did measure for snoring and I was snoring for something like 80% of the night, so really high. Can that have an effect on the quality of sleep as well as the apneas? I'm not too sure what RERA events are to be honest. I'll have a look into that and see if they showed up on the test. I'm not really against the idea of a mask/Cpap, I imagine it's something I could adjust to. I guess I'm just trying to figure out if an AHI of 8 is worth trying to treat. At first, I was a little dismissive as the notes of my study did describe it as very mild. However, when I have a day when I can't stay awake in a car or watching TV, it makes me wonder how much this is permeating into my overall quality of life, and if treated, would I feel better.
RERA Respiratory Effort-Related Arousal.
You have a right to a copy, a full copy, not just the summary, of your sleep studies. I do suggest that you redact it (no names addresses etc) and post it because all too often important details are not included in the summary or you do not understand the terms mentioned.
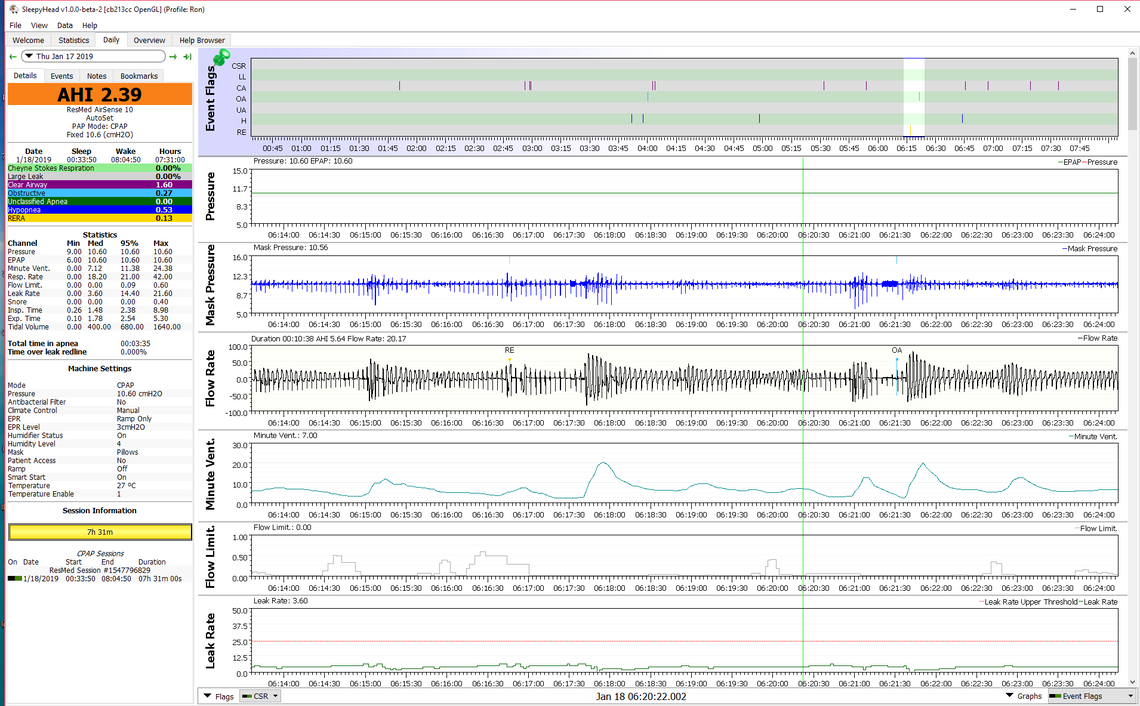
Yes, I think snoring does reduce the quality of your sleep. So does flow limitation and it is typically not reported other than when it makes the 10 second flow reduction to qualify as a hypopnea event. Here is an example of a RERA event I posted in another thread. It is from my data and it preceded a full obstructive apnea event. In this graph you can also see Minute Ventilation which is just a measure of the air (oxygen) being exchanged with your lungs. The reduction in air exchange was more significant in response to the RERA event (RE) than it was to the obstructive event (OA). So they do count as a factor in the quality of sleep.
Not sure how the PAP prescription process goes in your area, but here (Alberta, Canada) after a home sleep test which is positive for apnea, it is pretty standard to prescribe a free trial of a APAP machine, and after that if it is successful you can buy it from the clinic ($$$) or elsewhere on line ($). The good part about a trial is that you get to try one or more masks which is most difficult part in gaining comfort, and you also find out what the machine does for you.
The industry standard is to treat AHI>5. One issue with a home sleep test is that they base the AHI average on machine operating time, or possibly body in position (lying down) time. There are no electrodes attached to your head so they can't tell when you are asleep or not. The more time you spend lying down during the test but not sleeping, the more the home test underestimates the real rate of apnea and hypopnea. Your in lab test is most likely to report a higher AHI than 8 because of that factor.
Oh, this is very interesting! I actually remember sleeping very little the night I did my study. I was slightly surprised that I slept enough for them to draw any conclusions. So, am I right in thinking that this average isn't taking into account how much time I was actually asleep, so my AHI could actually be significantly higher?
You said no Central Apnea, any Mixed or Complex Apnea? These are really Central Apnea and Obstructive Apnea mixed or combined.
Here is a link covering soup to nuts targeted at the beginner at treating Apnea but also good info for those that are more advanced as well.
[http://www.apneaboard.com/wiki/index.php?title=New_to_Apnea%3F_Helpful_tips_to_ensure_success]
Thank you, I'll have a good read over this stuff.
Okay, after looking over the report again (It's been a few weeks) I actually had 0.3 central apneas per hour, 0.5 obstructive apneas, 0.2 mixed apneas and 6.3 hypopneas per hour. Totalling 7.3 per hour (AHI). Although as mentioned in my post above, I didn't have a very good nights sleep at all, which may have thrown these averages off if they don't actually measure when you're sleeping.
Here is a link to a study that looked at a number of people who were diagnosed with a full in clinic study, and then estimated what the AHI would be if Time in Bed (TIB) was used instead of Total Sleep Time (TST). It not unexpectedly showed that many who were diagnosed with mild sleep apnea (AHI 5-15), would have been missed and diagnosed with normal apnea levels (AHI 0-5). They reported it in a pretty complicated way, but the conclusion is obvious. The more differential there is between TIB and TST the greater the error in reported AHI.
Potential Underestimation of Sleep Apnea Severity with At Home Kits
My opinion is that there is not much wrong with a home test, as long as one understands the limitations. And with respect to RERA events even though they are likely to measure them with an in lab test, the large majority of of insurance companies will not count them in determine eligibility for coverage. For example AHI - 4, and RDI - 15, no coverage!
Hi Denzel
I don't think the sleep study processes are an exact science however you do them.
It's been years since I did a home study but I had a clear impression at the time that what the 'expert' did when he/she received the data from the device was simply select the highest density of apnea data and trimmed off the build up and trail off data before they started counting and measuring.
If that impression is correct then they can effectively 'see' when you were really asleep.
I presume there must be a minimum acceptable frame for such data but it may be as low as an hour or two.
I really should ask some of the more difficult questions.
How old are you?
Are you gaining weight?
Are you under significant stress?
Have you discussed other causes of fatigue with your doctor?
I am not implying that CPAP or dental devices would not benefit you because anything that disrupts your sleep will have cumulative effects, and snoring is a pretty strong indicator in itself, but your sleepiness symptoms seem excessive enough to suspect additional causes.
A path that you could use would be to get a trial use of a ResMed Airsense 10 AutoSet or AutoSet for her (which has an additional algorithm designed for women, thus skipping the in-lab sleep study.
Oddly the cost of an in-lab sleep study is ball park of the cost of the machine (actually the study cost is larger if the machine is purchased retail vs from a DME)
Hi Biguglygremlin!
I'm actually slim and healthy, by apneas are most likely caused by a recessed jaw and/or deviated septum. I would describe myself as someone that mostly copes with life/stress, but I have had a few battles with depression/anxiety, mostly circumstantial but I'm beginning to think that OSA might be behind (or at least exacerbating) a lot of difficulties. I feel like compared to the average Joe I've had to have a strict lifestyle to stay on top of things. For example, I rarely drink because I feel awful the next day, even after a couple. I exercise and eat a clean diet.
I've looked over all the data, and I can see that my AHI has been determined by time in bed (8.5 hours) but I know I slept far less than this. With this in mind, I'll book an appointment with my G.P. tomorrow.
Thanks everyone for all the useful information, It's been amazing as I can see how underestimated my AHI is. This makes sense because even though it showed very mild OSA, it didn't feel mild. Today I literally couldn't stay awake on a 90 minute bus no matter what I did!
Hi Denzel,
Since you are interested in quality of life, I wanted to let you know that when you complete the MyApnea research surveys, you get a report that shows how you scored on some quality of life outcomes like insomnia, sleepiness, depression, and daily functioning. Most of the scores are from validated screening questionnaires that your doctor or medical researchers might use. Given your questions, I thought you might be interested in this resource.
Best of luck!
I found a bit of info on how apnea is dealt with in the UK. I think the good news is that if you are formally diagnosed they give you a machine on trial for free essentially for a month and you get to keep it if it works. Not sure how much choice you would get to what kind of machine it would be though. Getting diagnosed might be an issue too. See this link on Diagnosis. The last paragraph is a bit concerning and says:
"Current evidence suggests treatment is most likely to be beneficial in people with moderate or severe OSA. However, some research has suggested treatment may also help some people with mild OSA."
Since you are in the mild category for severity, I'm not sure where that leaves you. Perhaps there is discretion if daytime sleepyness is a big issue. But, it may kind of depend on where you want to go with it. If you want PAP treatment and it needs a Moderate severity to get one, then you would probably want to push for a in lab sleep study, as it most likely will result in a higher AHI.
It also appears you may have some choice in where you get your sleep study done. I believe this is a list of approved clinics and hospitals. Perhaps one thing you could do is "shop around" and see if you can find out what machines they would fit you with if you meet the diagnosis criteria.
There are some medical studies that question the efficacy of treating mild OSB sleep apnea with CPAP or APAP. "Mild Obstructive Sleep Apea Should Not Be Treated" by Michael R. Littner, MD. Journal of Sleep Medicine, 15 April 2007 ABD. It is available on the National Institutes of Health website.
Here's a tip about reading medical studies. Be sure to check and see if they are funded by or otherwise connected to corporations. This information will be in the Disclosure Statement. If they are connected to corporations use the information they present with great care.
Yes a very interesting article Muley Mild Obstructive Sleep Apnea Should Not Be Treated {Link to above article.}
It's a view that should be broadcast and applied as fully as possible.
I believe that not just medical or surgical intervention should be applied to Apnea below 20 but also urgent education and training as well as any other kind of intervention that could help people to manage their lives more effectively without resorting to a lifetime dependence on CPAP machines.
It strikes me that making a recommendation that mild sleep apnea (5-15 AHI) should not be treated, is like saying those who smoke 15 cigarettes a day are in no danger of getting lung cancer. It could be true. Or it could not be true. And you only know for sure when you get lung cancer, or die from something other than lung cancer.
I've generally agreed with your position on most things Sierra but I guess there is a time and place for everything, including dissent. :P
Despite it's misleading title the article does not actually recommend that Apnea not be treated but suggests that it would be better if it were treated by a range of alternatives to CPAP.
I could be wrong here of course but isn't it true that OSA is normal in the population and so Apnea is not diagnosed below 5 events per hour.
Wasn't this number reached in conjunction with capitalist organisations and marketing companies who depend on sales and other aspects of the sleep industry for their income stream along with 'authorities' who depend on statistics to justify credibility, power and funding.
If those interests were involved in choosing a level of OSA to be deemed normal and their motives and goals are clearly self serving what would be a truly normal range?
If we are not prepared to put all humans on air or oxygen therapy where do we draw the line?
More importantly and relevant to your comparisons WHO do we trust?
I must admit to feeling that there is a large dose of wisdom in the above admonition from Muley to look closely at the disclosure statements and even then add a generous pinch of salt if you are as skeptical as I am because everybody has multiple agendas. (I note that you yourself have often raised a caution related to research results that are industry funded)
I certainly believe that something should be done about mild OSA.
Not just something but a whole range of things.
I feel quite strongly that if we are to find solutions to Apnea then nearly ALL the focus and help needs to be directed to those with mild apnea with the goal of preventing it from deteriorating into more serious Apnea.
CPAP is Not The Solution(says me with very severe Apnea who is totally dependent on CPAP)
CPAP It is a form of surrender.
CPAP seems to me to be a very lazy and shortsighted approach especially when it comes to treating mild Apnea.
Even if your prophecy of pending doom for mild Apnea sufferers should prove true surely many other options could have been applied before resorting to CPAP
Well that is my feeble attempt at a dubious victory. It was worth a shot though wasn't it? :)
You are invaluable to this forum Sierra and a source of hope and confidence to many despairing CPAP users.
I admire your precision and research capabilities.
I'm just a stirrer who plays with the abstract and philosophical angles.
I may sometimes be right in principle but there is little doubt that you are right in practice.
That doesn't mean that I have to like it though! :P
I hear what you are saying, but I am not a big believer in conspiracy theories. Every once in a while you hear that big oil companies have a secret safe where they keep all of the 200 mile per gallon carburetors, and engines that run on water instead of gasoline. I think the reality is that we would not have for example the medications we have today if the drug industry did not fund the studies to prove they are safe and effective. It is government regulations that force them to do that, and they have to comply to get approval to market the drug. Yes, there have been studies which have exaggerated the benefits, and claims made that have proven to be false on closer examination. There is the example of the former British doctor Andrew Wakefield who published a study claiming MMR vaccine caused autism. It has since been withdrawn.
I think one could also make the argument that the UK National Health Services and their doctors are not totally unbiased. In the UK CPAP is a covered medical condition. They pay for the studies and the CPAP equipment. One could say that they are motivated to minimize the cost to the NHS. The UK not unlike Canada and Australia operate more of a "best buy" system of health care. Our costs are in the order of half what the US spends per capita on health care. And the ironic part is that being the highest per capita spender on health only puts the US in 45th position by country for life expectancy. I recall a while back that the UK restricted availability to heart bypass surgery, because they believed it it did not on average extend life. The UK are about 30th on the life expectancy list, while Canada and Australia are closer to 10th. Perhaps they are cutting a little too close to the bone in trying to save health care costs?
I think that a mild diagnosis of sleep apnea is not unlike pre-diabetes. Yes there are different ways of treating it and losing weight is a good idea for many reasons. Studies show the metformin which is a very inexpensive drug does a good job of reducing A1c, and often helps with weight loss. Is it needed for life? Sometimes yes, and other times no, and lifestyle changes addresses the issue. But to me withholding the metformin makes no sense. This is like apnea. If the individual has sleep issues, wants to try CPAP, and in many cases is willing to pay out of their pocket for it, then why not do it. The only risk I see is that if the discomfort factor of using one outweighs the apnea reduction benefit, then it may not be a good idea. Contrary to what that doctor claimed it is hard to imagine many cases of obstructive apnea at 15 that would not be improved with PAP treatment. The real question may be if there is an improvement in sleep quality, and is that improvement cost effective? The answer may be in the eye of the patient and the one that is paying for the treatment if it is not the patient.
Denzel, Treating my apnea (AHI 8) has resulted in better concentration, and heart issues went away. So, treating mild apnea can result in better quality of life.
Much of the above discussion is not about Denzel specifically but about the bigger picture of best practice for treating mild Apnea.
Muley, and I, as well as the research paper he referenced, all tried to make a point that has been totally missed or misconstrued.
At no time was it stated or even implied that mild Apnea should not be treated.
The question was never if it should be treated but how it should be treated.
The reason I am still hanging around this forum is embedded in this issue.
I believe that CPAP is an irresponsible, short sighted, lazy way to treat Apnea when there is still a potential, in mild cases, to develop and apply real solutions with the hope of turning the situation around and enabling lasting lifestyle changes.
I think if we were socially and morally responsible we, the ones who are already condemned to depend on these machines for the rest of our lives, should be doing everything in our power to direct people away from CPAP dependence and towards REAL solutions that would enable them to avoid our mistakes and the circumstances that have entrapped us.
In my view all the funding, research, educational campaigns, expertise and help should be directed towards prevention and cures for those with mild Apnea and not focused on hooking them all up to CPAP machines.
Despite all the views one way or another on SA treatment (or non-treatment) for right now it comes down to this--CPAP is the most effective, least invasive and most affordable treatment there is. Not in all cases but most. Yes, we need to be educated on ALL options and even more on ALL ways that we can help ourselves by changing our lifestyles. How many people do that? Very few.
For most of us, oral appliances or implanted devises are not covered by insurance. Implants have a whole 'nother set of issues associated with them. That does not mean that we just accept the CPAP as the end all/be all but that it is what we have.
So what needs to be done? We need to advocate for better outcomes and therapies. Is that easy? Of course not. For one thing we are sleep deprived and face other health issues. When we don't, then I agree--laziness or apathy keeps the status quo. Speaking in generalities here--if you see a problem, do something about it. Join an advocacy group, write letters, make your voice heard.
Gremlin, I agree 100% that all the funding, research, education, etc. should be focusing on prevention and cures as well as better treatment options. But that's not where the money is. Research cannot happen without funding and funding goes towards CPAP more than anything because despite it all, that's what people are directed to. Should doctors be more proactive with this? Of course! Maybe we need to push them, I don't know.
Long-winded I know and lots to wade through and totally my opinion.