Hello all,
Here's my story so far. Recently I am having sleep transition issues where I would wake up gasping as I was about to fall asleep. This would happen several times at night , and would leave me awake for hours at a stretch. I had a sleep study done on recommendation from my doctor and results are still awaited. Searching through the net, I found something called sleep onset central apnea , which seems to fit my symptoms.
I also came across many articles , which seem to suggest that these are a part of normal sleep transition. My question is : How can they be normal when they start interfering with your normal sleep cycle? How do people cope with it? As expected, the following day, I am quite sleepy and tired and have to take repeated naps during the day. This is beginning to affect my work..
What are the best options for sleep onset apneas( not OSA or CSA which occurs once you are asleep)? Do sleeping pills help? Many questions.. Any suggestions/remedies welcome.. Please help me overcome this nightmare
I have heard of this issue, and as you say it is considered more of a nuisance than a serious medical condition. I think it is a basically a change of shift problem. The day shift guy that is controlling your breathing goes home before the night shift guy takes over, to put it in analogy form.
My thoughts would be to wait until your sleep study results come in. For sure ask for a written copy of the study results as there is a lot more detail on the report than can be remembered with just a verbal discussion. If the conclusion of the study is that you have sleep apnea that needs to be treated with a CPAP, you might get some relief from the therapy. A CPAP addresses obstructive apnea by keeping the airway open with pressure. With a central apnea there is no obstruction, so pressure does not help. That said, if you have the right kind of machine, it can provide a split in the pressure supplied during inhale and exhale cycle while you are going to sleep. That MAY help prevent your issue of stopping breathing when you are going to sleep. I am a CPAP user not a medical professional, so that is just my opinion. And my opinion again about machines is that the ResMed AirSense 10 AutoSet does the best job of the getting to sleep phase. It lets you use this split pressure (Expiratory Pressure Relief - EPR) while you are awake, and then when the machine detects you are asleep it stops the EPR. Treatment during sleep can be more effective with EPR off.
You should also ask your sleep clinic that did the test what they think of your condition and might improve it.
Thanks .. Other than AirSense Resmed 10 are their any other CPAP/BiPap machines which help with sleep onset apneas? I have heard there are some machines which automatically detect absence of breathing for a set period of time and start it if absent. I also probably have mild OSA as per my sleep report( Though not official , i had a chance to peep into it as the tech was preparing it). The machine needs to be portable as well as O travel sometimes
The AirSense EPR is probably not really intended to assist in breathing stoppage as its main purpose. It is unique in that it can use EPR during the going to sleep and then turn it off when you go to sleep.
The next step up from an APAP like the AirSense is a Bilevel like the AirCurve 10. There are various models but what it provides over the AirSense is the ability to provide more than 3 cm of EPR or Pressure Support as it is called on a Bilevel. With a higher differential between inhale and exhale it can assist breathing more when the person is not doing it themselves. Depending on the machine this pressure support can be variable in that it detects when you need more or less pressure support. In the AirCurve line there are some that have a S mode which provides a back up breathing assistance at I believe a fixed 25 bpm when it detects no breathing. These machines also have some settings that let you control how the switch from inhale to exhale pressure to fine tune the breathing assistance.
Then there is the AirCurve 10 ASV model which is an adaptive servo-ventilator machine. It monitors every single breath and assists on a breath by breath basis to maintain breathing. Here is a link where you can find more info on the various options. It is pretty high level however, and you have to get into the technical manuals to see what they really can do. Phillips Respironics probably have similar capability machines. Sometimes the bells and whistles differ a little.
When you get your sleep report you should discuss these options. However if your apnea is in the mild category, they are not likely going to want to consider anything more than an APAP. In that category I would recommend the ResMed AirSense 10 AutoSet for Her. The For Her version as an additional option mode which may be of use to a male or female, and the price is the same. You can select the For Her mode, or standard APAP mode.
On portability the standard AirSense model is quite portable, and what I would recommend using. They come with a nice carrying case that holds everything you need, and has a strap to attach it to the top of a rolling bag. We have a Z1 Travel Auto CPAP but don't use it, as it has too many compromises for my liking. In my view, a travel CPAP is a solution in search of a problem. A CPAP is considered a medical device and you can carry it on a plane in addition to your normal carry on limits. That is why it is handy to have one that attaches to your carry on rolling bag.
Hope that helps some,
Thanks for the responses. I called up the sleep medicine center and they said results would take upto four weeks! four freakin weeks! I spend upto 4 hours every night tossing and turning without sleep. I can't wait that long.. Do sleep meds help ? (I have already tried melatonin , no use). Should I ask my doc to prescribe some pills? Thanks.. and sorry for the rant..
I would guess that it is OSA. Let me ask you this, Did you gasp for breath when you woke up, do you snore and did you feel your throat move when you woke up? Think about it. OSA does hit you when you are falling asleep, I used to notice it when falling asleep. Just starting to sleep, then the next you know is you waken up with a start and gasp for breath. There is also another thing that can happen, you slowly slow down with your breaths, then they get shallower until you stop breathing altogether, but it is not normal to wake up gasping, more you just get a start and start to breath again, this is more like CSA. I used to do this as well, but I didn't get a so big a gasp of air, but breathing did quicken until it caught up. OSA can leave you gasping, hart racing and a bit confused. I would wait until you get your results. If you do have OSA, ask for your report so you have a copy of your results. If you can get an APAP machine, these adjust to the pressure you need and are a lot better. You will have to work on thet one, ask your doctor to give you a prescription for an APAP.
I would think so but I dont normally snore so it makes me think these are mostly sleep onset CSAs. During my sleep study the technician did tell me that I had mild OSA but I am not sure if these are playing up at sleep onset or are they Sleep onset CSAs.
I dont seem to have any 10 second breathing pauses normally associated with csa.
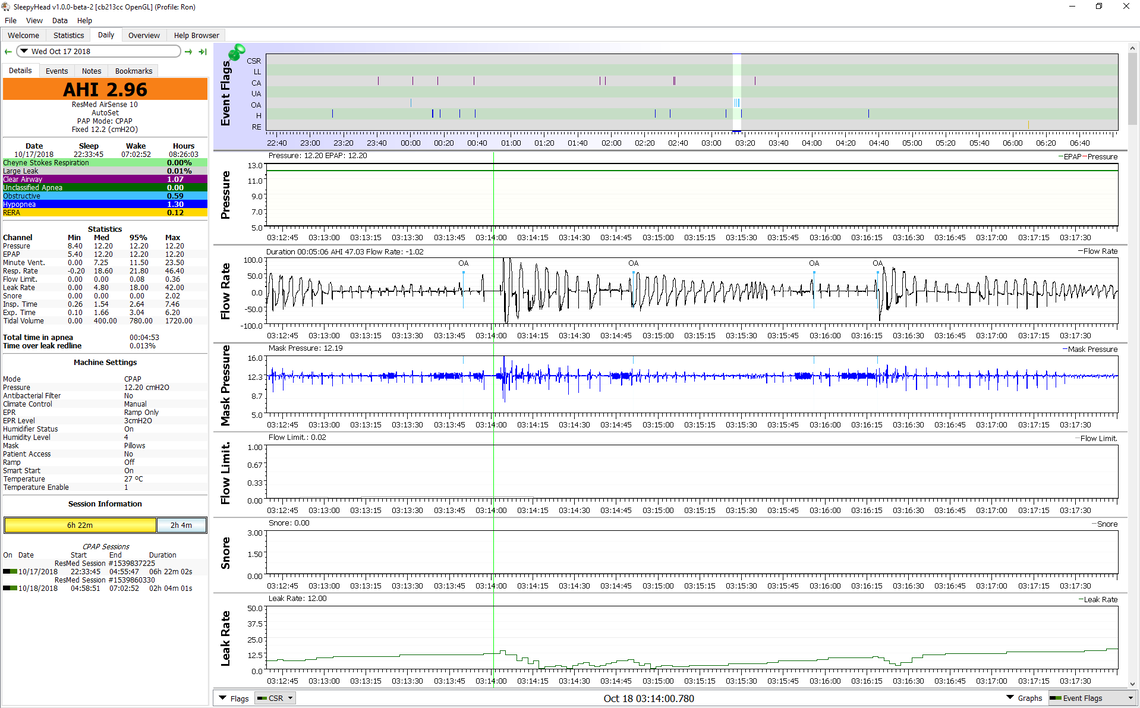
This is what obstructive apnea looks like in a SleepyHead report when it occurs. Last night I had a series of 4 OA's in quick succession. After the first one in particular you can see the wild flow rate fluctuations and mask pressure fluctuations. Mask pressure is set at a fixed 12.2 cm, but it went as low as 8 cm and over 16 cm. I was probably gasping for air. Keep in mind that you can have an apnea just when you are going to sleep, not just when you are sleeping.
Ok learned folks.. Had an appointment with the sleep doctor about my sleep study. My AHI was 19.6 , which puts me in the moderate range, I guess. What surprised me was that out of a total of 104 events in 5 and a half hours of sleep , 103 were hypopneas! There were 0 OSAs, O CSASs and 1 mixed apnea event. The doctor advised me for a CPAP titration study. I do have the following questions for the learned members: 1) Is there any way to know if these hypopneas are central or obstructive, since the report does not tell about it? The doctor was fairly confident that these are obstructive in nature , since I don't have underlying conditions for a central. 2) What to expect during a CPAP titration test , since I am quite apprehensive about it? 3) What kind of CPAP device will be best suited for my condition ?
Thanks in advance for the wonderful website and support!
1) Is there any way to know if these hypopneas are central or obstructive, since the report does not tell about it? The doctor was fairly confident that these are obstructive in nature , since I don't have underlying conditions for a central.
One would have to look at the breath by breath flow charts to see what is happening. In my experience looking at results on SleepyHead a hypopnea can be either central or obstructive. If you are getting a waxing and waning of breathing depth in a smooth cycle that does end in a full apnea, then that would suggest a central event. And I would think during the sleep test they would monitor not only the flow but your effort to breathe. Central apnea is basically a reduction in effort to breathe. Perhaps the doctor has looked at that when making the opinion.
They should be able to tell during the titration test though. If increasing pressure does not resolve the hypopnea then that suggests they are central in nature.
2) What to expect during a CPAP titration test , since I am quite apprehensive about it?
If you had an in lab sleep test it should be very similar to that. They will just increase the pressure over the night and find out what is required to resolve your hypopnea. They will also be checking for any indication that increasing pressure causes central apnea events.
3) What kind of CPAP device will be best suited for my condition ?
If pressure resolves your hypopnea, then the two obvious choices would be a fixed pressure CPAP, or an APAP. I push as much as you can for an APAP that saves detailed data to the SD card. You don't want to get stuck with a fixed pressure "brick" that gives you no data to monitory your results. I would push for the ResMed AirSense 10 AutoSet.
Now if the pressure does not resolve your hypopnea because it is central in nature, then an APAP may not work that well. The other choices would be a BiLevel machine or ASV. Probably a bit premature to be considering them at this point though.
Thanks agai My main apprehension is about wearing the CPAP mask and adjusting to it. Will it be too suffocating? What happens if the pressure is set too high?
During my first sleep test I had all the wires hooked up but no mask. I guess it is goi g to be a challenge sleeping with the mask on
Some things to consider. The sleep technician is going to spend some time with you to fit you with the best type of mask for you, and ensure it fits you well without leaks. The test is normally started with the lowest pressure, and then over the night it is increased to find out at what point your hypopnea is normalized. My expectation would be that you will not go to very high pressure as you are not experiencing full apnea, but there is nothing real predictable about CPAP so you never know for sure. And as far as the suffocating feeling, you are more likely to find it easier to breathe with the low to intermediate pressures. I consider the pressure my friend! They need you to be asleep to monitor apnea events, so the pressure is going to be increased when you are asleep and you are very unlikely to notice it, unless you wake up. I presume then, they will back pressure down and wait for you to go to sleep again.
I find the main issue with wearing a CPAP is the comfort factor of having to find a place on the pillow where the mask is not going to be dislodged, and a location for the hose that is not in your way, and you are not sleeping on top of it. You have to be able to change sleeping positions with some ease. And, of course they know all that, so they will help you get that sorted out.
I would focus on just relaxing and getting as good a sleep as possible under the circumstances.
Simply put, there is no such thing as a central hypopnoea. Hypopnoeas are not actually classified as obstructive or central, they are just hypopnoeas, so I wouldn't worry about it. A better question is "does CPAP get rid of them?", which a titration study will tell you.
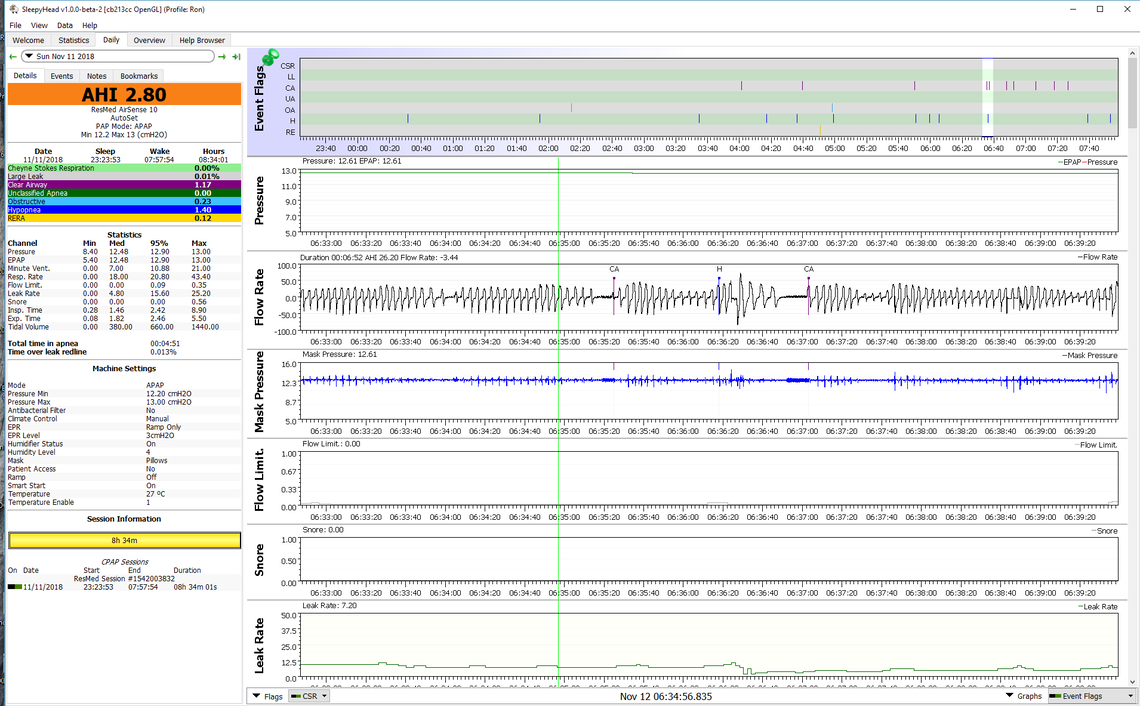
Sorry, but I can't agree with you on that one. I see hypopnea all the time in my SleepyHead that are clearly central apnea issues that do not go fully to an apnea or breathing stoppage. Here is an example. You can see a CA event, a second CA event in formation but not going to a full CA and is identified as a hypopnea, and then another CA event. They are all part of the same unstable breathing control system that causes my CA. These type of hypopnea are not resolved with more pressure.
I think you may be misunderstanding what I wrote. Whilst your hypothesis as to the cause of your hypopnoea is interesting it doesn't change the fact that, in medical terms, there is no such thing as a "central hypopnoea" because hypopnoeas are not classified as either central or obstructive. It's all down to the rules for scoring sleep. Apnoeas events are classified as either obstructive, central or mixed. Hypopnoeas are not. They are just hypopnoeas and don't come in different varieties. While we may make an informed guess as to the cause of a hypopnoea, it will always simply be classified as a hypopnoea because that is all the rules for scoring allow for. One day they may be modified to expand on this point, but until then we are stuck with only the one type of hypopnoea.
Sleeptech, this one you are wrong about. Central Hypopneas are optional to report from a sleep studies (I have yet to see one that does.) They are part of the criteria that medicare uses when determining qualifical=tion for bilevel with backup. here is the definition.
[https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3459210/]
towards the bottom.
Hypopneas - Obstructive and Central To determine the statistics for Central apneas and Central hypopneas >50% of total AHI above we need to determine which hypopneas are central in nature. The description below defines the difference between obstructive and central hypopneas.
An obstructive hypopnea contains one or more of the following:
An increase in PAP flow signal Snoring during the event Paradoxical breathing A central hypopnea will have none of the above.
Central Hypopnea. Central hypopneas are associated with reductions of purely in-phase thoracic and abdominal effort or movement signals, followed by an increase in chest and belly movements at the end. There is no evidence of phase shifting or paradoxical breathing, no airflow flattening, and no snoring throughout the entire central hypopnea.
A Central AHI is composed of Central Apnea and Central Hypopnea. The Central Apnea numbers are easily extracted from modern PAP machines which report detailed efficacy data. We need to concentrate on Central Hypopnea numbers to demonstrate a Central AHI >5 and that Central apneas and Central hypopneas >50% of total AHI
Central Hypopnea. Central hypopneas are associated with reductions of purely in-phase thoracic and abdominal effort or movement signals, followed by an increase in chest and belly movements at the end. There is no evidence of phase shifting or paradoxical breathing, no airflow flattening, and no snoring throughout the entire central hypopnea.
Paradoxical Breathing explanation: The chest and abdomen should expand when they inhale and contract when they exhale. If the chest and abdomen contract while inhaling and expand while breathing out, a person may have paradoxical breathing.
I can't agree either. When I was diagnosed in the UK, the Sleep Doctor (A Professor) sat down and explained OSA, CSA and Hypopnoeas. Yes CAs and Hypopnoea might be related, but they are not the same. He went through my data in detail and he pointed out the three types to look out for. His next words were "Do not play around with the settings!" "Yes Doctor" I said as I was already working out how to do it. He took the manual from me, but I sent away for another. He knew fine I was going to get the best out of the limited machine I had, I did as well. As machines got better so did the treatment. But he didn't keep the manuals from me after the second machine. There was little or no internet back then, or Sleepyhead. It took me a while to get an Internet connection worth using, it was very slow, but at least the modems had evolved by then. Dial up! Slow Dial up at that.
I think you may also have misunderstood what I wrote. I certainly didn't suggest that hypopnoeas and central apnoeas are the same thing. See my post above for an expanded explanation.
There seems to be some recognition that both central and obsructive hypopnea events do occur although they may be difficult to classify. See this page from a sleep report posted by another contributor here. The columns for Central Hypopnea and Obstructive Hypopnea were not filled in, and they were all recorded under Unclassified Hypopnea.
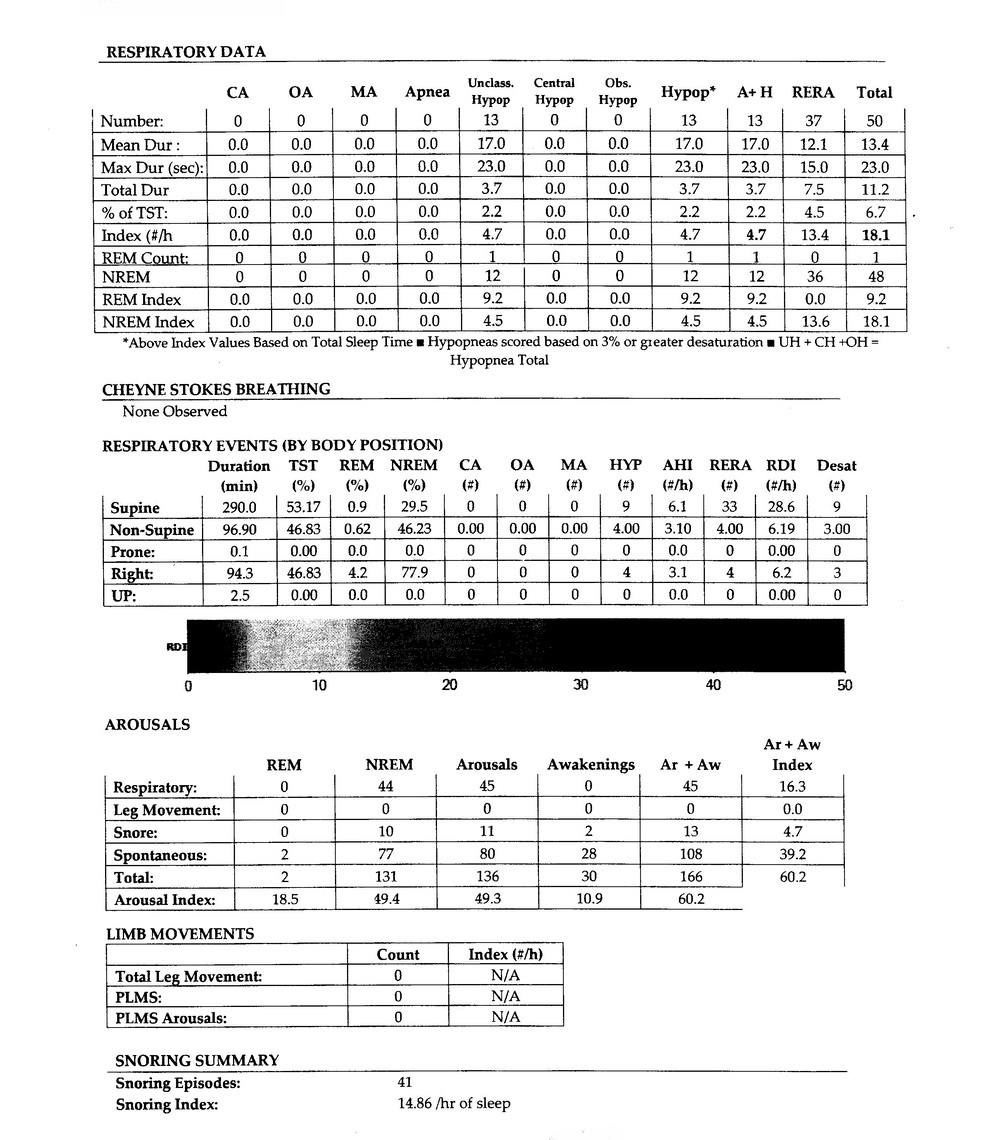
Also see this article.
The fact that there are columns just means that whoever was laying out the document was ill informed. The international standard rules for scoring sleep only allow for hypopnoeas, not obstructive hypopnoeas or central hypopnoeas. The columns doen't change that. Neither does that article. Whilst the theory is interesting enough, they will all get scored as hypopnoeas until the rules change.
It is also possible that some labs may decide to ignore the rules and do their own thing. That happens sometimes. Unfortunately it means the data they collect is no longer comparable to other data which does adhere to the standard rules.
Ok folks.. An update on my situation. I finally had the first taste of an xpap machine at the sleep lab. It was not as bad as I thought it would be. I slept about 5 and a half hours during the test which is not bad as per my standards, though the mask kept slipping constantly and i had to adjust it through the night. A couple questions for the pundits:
1) the machine used in the sleep lab was a resmed vpap. Is vpap same as a bipap? Does it help with sleep onset apneas/ hypopneas?
2) people and experts say sleep onset centrals are normal. How come I wasn't experiencing them before and now suddenly its an issue?
As usual , thanks to this wonderful forum, in particular Sierra and sleeptech for their wonderful insight and knowledge. Without this forum, I would have felt alone in this battle.
In the absence of any further detail, my suggestion would still be to push for a ResMed AirSense 10 AutoSet For Her version. It has an optional For Her mode in the machine that is better for treating hypopneas and RERA events. It also has the advanced features that can be set for getting to sleep.
Here is a link that provides a deep dive into how a titration test is done and the various options for treatment. But, at this point it would be really helpful to get more detail on what the outcome of the titration test was. At this point I don't see anything that would suggest you need a AirCurve BiLevel or ASV type of machine.
Getting back to your issue of apnea right at sleep onset, that could be either central or obstructive. Your muscles relax when you go to sleep and it is quite possible that your upper airway constricts to reduce flow or even collapses stopping flow as you go to sleep. Since your sleep report had no central apneas reported, it seems more likely that it is obstructive. It would be helpful to know if any centrals were detected during the titration test, as the pressure from the test can produce central apneas.
But, assuming the more likely case of it being obstructive in nature, and that the hypopneas are a flow reduction due to upper airway restriction, a PAP device is likely to address the issue. If you get the pressure in the airway up BEFORE you go to sleep it is much less likely to have the airway collapse when you do fall asleep.
The next step should be to get a trial machine and see what the machine can do for you in actual use at home. It would be most efficient to get a flexible machine like the ResMed For Her AutoSet, as it can be set up to get you to sleep in a few different ways, which you could try to see which works the best. They would be:
In other words lots of options to try. I suspect one of them will work for you.
Ok .. I got the prescription for a CPAP with a pressure of 10.. Now if I get a ResMed 10 autoset for her for what amount of time should I set the ramp for? Also, is a pressure setting of 10 high or low? Excuse my ignorance in this matter
A setting of 10 is moderate. The machine is capable of going from 4 cm to 20 cm. I am now using a pressure of 11 cm. If you are going to run the machine in the For Her Auto Mode, and your recommended fixed pressure is 10 cm, I would set the minimum pressure to 8 cm, and the maximum to 11 cm as a starting point. Then after some experience with that setting and using SleepyHead to monitor the results, you can either refine those pressures, or go to a fixed pressure based on actual experience with the machine. Here is a cut and paste copy of what I gave another user of the ResMed for initial setup for comfort.
A little further down on the setup menu under Options you will find this item:
If the issue of apnea events right as you go to sleep is not solved by this, there are other options. But I would start with this.
I find with EPR at 3 on ramp only I find a ramp start pressure up to 8 or 9 quite comfortable.
If you set the ramp type to auto it will stay at the ramp start pressure until you go to sleep, 30 min max. The for her mode is more responsive to hypopnea, and less to apnea. And if it does not work well in the for her mode, you can just switch it to standard mode.
Going through this, one question popped up in my head. How could a hypopnea possibly be central?With Central sleep apnea you are either breathing or not breahing at all.Is there something like partial breathing? Like a partial airway closing in case of obstructive hypopnea .
Sorry, but I missed this post. The difference between a central hypopnea and an obstructive hypopnea is the breathing effort. With obstructive hypopnea there is normal or even increased breathing effort but reduced flow due to a partial obstruction in the airway. With a central hypopnea there is simply reduced effort to breathe with no obstruction. With central apnea it is quite common for breathing effort to go in waxing and waning cycles. Your body is having trouble with the control system which is designed to keep oxygen and CO2 levels relatively constant. If this reduced breathing effort continues for longer than 10 seconds with flow less than 50% it gets flagged as a hypopnea event. The machine however has no way to distinguish if it is due to reduced effort or due to obstruction, so it just says hypopnea.
So finally I got a prescription for a CPAP machine. I didn't get a copy of it so far , which will be sent directly to the medical equipment supplier. My CPAP trial begins early next month. The recommended pressure setting is 10 .. Is that a high or a low ? Also, if I use Resmed Airsense 10 with autoset for her, at what pressure should I start at the ramp and how long so the ramp be set for? Excuse my ignorance in this matter and thanks again
I answered most of this a bit further back in the thread. Here is a copy.
A setting of 10 is moderate. The machine is capable of going from 4 cm to 20 cm. I am now using a pressure of 11 cm. If you are going to run the machine in the For Her Auto Mode, and your recommended fixed pressure is 10 cm, I would set the minimum pressure to 8 cm, and the maximum to 11 cm as a starting point. Then after some experience with that setting and using SleepyHead to monitor the results, you can either refine those pressures, or go to a fixed pressure based on actual experience with the machine. Here is a cut and paste copy of what I gave another user of the ResMed for initial setup for comfort.
A little further down on the setup menu under Options you will find this item:
If the issue of apnea events right as you go to sleep is not solved by this, there are other options. But I would start with this.
Here is a link to a video on how to set the AirSense 10. I would also download SleepyHead so you can monitor the results you are getting from day 1. The settings may have to be adjusted a little based on your actual experience with the machine. Another poster put some examples of SleepyHead reports a little further back in this thread.
You for sure want to get a hard copy or pdf copy of your sleep report. You will want it for future reference as to where you started this CPAP journey, and if you ever want to buy even a mask, you need it in the US.
In your first post you reported that you were having sleep onset apnea. I would hope that with the settings I gave you the initial ramp start pressure would be high enough to prevent the apnea. It it doesn't post back and there are some other options you could try.
Hi Sierra Another quick question. I forgot to mention that a lot of RERA arousals were detected ..There were many such RERAs during sleep probably caused by sleep onset apneas/hypopneas. What airsense 10 settings would help with those? Should I completely eliminate the ramp and go for the recommended pressure right away? Thanks again
I get some RERA events flagged in my sleep. I have seen no indication they are linked to sleep onset apneas or hypopneas. When ResMed flags a RERA event it seems to be associated with flow restriction and flattening off of the top of the inhale breath flow rate, and an irregular breathing event signalling an arousal. If you end up getting an AirSense 10 AutoSet For Her, it is especially set up to respond to RERA flow limitations, and snoring.
I would still set up the AutoRamp as I described in the post 14 days ago first. If it does not stop sleep onset apneas, then there are the options I also described. In other words set it up for maximum comfort first, and if that does not work, then try the other options.
Finally got the Resmed Airsense 10 autoset for her trial machine today. Got the Resmed airfit N30i nasal pillow mask as well. Seemed comfortable when I tried it out at the medical supplies store. My prescribed pressure is 10cm and ramp is set to 5cm for 45 minutes.
Fingers crossed as I start my CPAP trial
Get Sleepyhead so YOU can look at the details of what is going on. You will need an SD card if one is not already in the machine. \I do suggest trying auto mode too while you have the machine.
I will after my trails are over. Right now I am not allowed to tamper settings on the loaner machine used during trails
They will never know that you have taken the SD card out and copied the data to SleepyHead. Just put it back in after you have copied the data to SleepyHead. If there is no card in it. Just use any SDHC card from 4 GB to 32 GB. My thoughts are that the data is your personal data, and you should have it. If there is no SD card in it, then no detailed data will be saved, and nobody will get to see it. Not you, not them.
If your prescribed pressure is 10 cm, I would ask them to switch the machine to an AutoRamp with a start pressure of 7 cm. 45 minutes is way too long for most people. I'm generally asleep in 15 minutes. In AutoRamp mode it will keep the pressure at 7 cm until you go to sleep and then ramp up to 10 cm. Also ask them to set the EPR to 3 and for Ramp Only. What that will do is give you 7 cm on inhale and 4 cm on exhale while you are awake. Most find that very comfortable. Easy to breath in, and easy to breath out. Only 5 cm can feel suffocating.
Hi Sierra
I set the ramp to 30 minutes. Seems to fine so far. I also changed my mask to a Respironics Dreamwear full face mask. I noticed a few leaks sometimes as I am a side sleeper and the mask gets misaligned sometimes. Has anyone used mask liners to prevent leaks.? Any other tips to reduce/eliminate leaks?
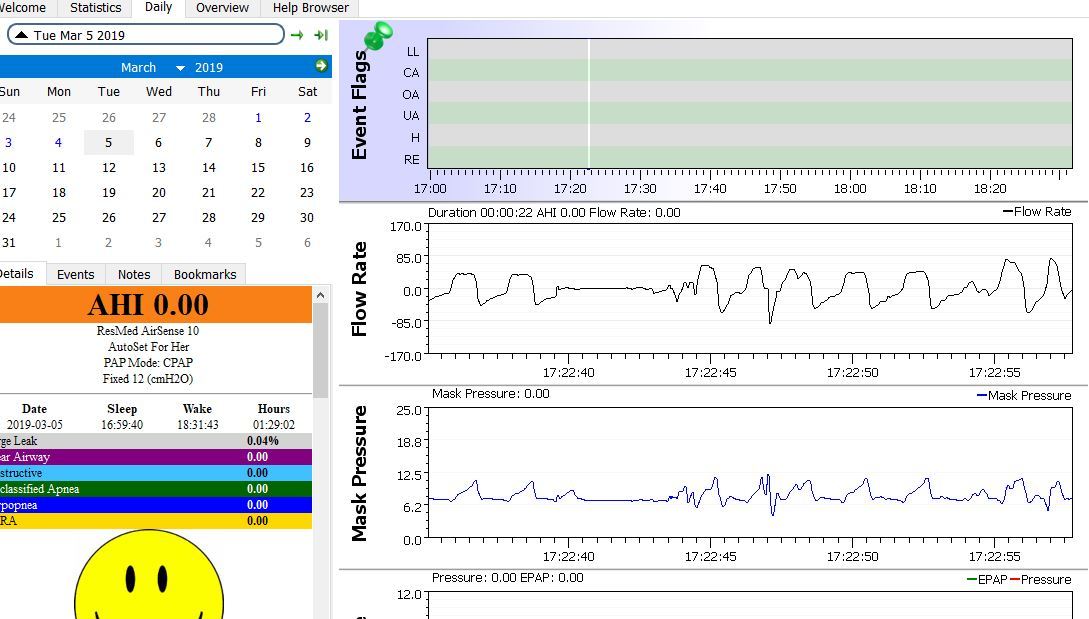
Ok folks . Time for an update. I am now into my 3rd week of CPAP trial and my AHI is down to below 1 and I am adjusting well to the respironics full face mask on resmed airsense 10 which is good. But what I don'tr understand is I am still getting sleep onset apneas which are not flagged as events either by resmed or by sleepyhead because they are less than 10 seconds in duration. One such example is shown in the image above. These onset apneas are the ones that sent me to the doctor in the first place. If I tell the doctor, he will simply dismiss them as being insignificant since they are less than 10 seconds. Any way to resolve this? BIPAP or ASV perhaps?
Could you expand the scale out some so I could see what the graphs look like leading up to the point where breathing stopped? What I am seeing is that you have the machine set at a fixed 12 cm, but the section you included has the pressure going up to about 12 cm but ramping back to 9 cm or so on exhale? I'm thinking you must have the EPR on and set a 3? If so, the first thing I would try is turning the EPR off. The flat top on the inhale cycle prior to the event may indicate flow is being restricted due to a partial obstruction of the airway. Once the flat tops on the inhale cycle and the short obstructive events stop, then you may be able to reduce the pressure some.
It is hard to tell how your machine is set because the whole calendar for the month is showing. If you click on that little black triangle beside the date it will hide the calendar and make more room. Also, if you go to File, Preferences, Appearance and uncheck the box that says show the pie chart, it will get that out of the way too.
The question is are these events significant?
Well, how do you feel? What are your symptoms?
Your numbers are better than excellent.
How you feel could lead to a change in treatment.
You can use SleepyHead / OSCAR to look at minor events. Click on Files/Preferences/CPAP check the Custom CPAP User Event Flagging checkbox and adjust the values for what you want to see, perhaps 80% and 3.5 seconds. You will have to play with that.
Do any of those events lead to an arousal? an SPO2 desat? How many of them? That one looks like you may have turned your head.
An isolated event like the one you captured is not significant. It would take a number of then close together ending in multiple arousals thru the night to bre significant.
Here are some Symptoms Note that these are not all specific to Central/Mixed/Complex apnea. They are symptoms that impact our sleeping, arousals, and yes apnea too. Think of these, but do not limit yourself to these when you are asked "How do you feel?"
Daytime hypersomnolence; Excessive fatigue; Morning headache; Cognitive dysfunction; Dyspnea, etc.; Fatigue; Insomnia; Difficulty going to sleep; Difficulty falling asleep; Wakening during the night; Daytime Sleepiness; Excessive Daytime Sleepiness (EDS); Poor concentration; Difficulty with balance; Shortness of breath; Dry mouth; Restless Sleep; Non-Restorative Sleep; Snoring; Obstructive Sleep Apnea; Restless Leg Syndrome; Nocturnal Leg Cramps;