Hi all,
I had an at home sleep study done on March 27th, 2020. My pAHI was 16.7.
I started using a Philips Respironics DreamStation AutoCPAP and was hoping to be pointed to resources that could help better direct my apnea management.
So far I have installed the Sleepy Head application to my laptop and have been generating statistics and reports with it, with little background knowledge of how to interpret the data to better direct my therapy.
I am trying to lower my AHI and get the best, uninterrupted sleep possible.
Thanks, Jason
Hi Jason,
A good starting point would be to post your typical Daily Report screen from SleepyHead. That gives the best snapshot of where you are. On a PC you just maximize the daily report and press F12 to capture the screen shot. In the bottom right of the screen a pop up will let you know where it is saved. With File Explorer just left click on this file and drag it into the body of a post. It should upload. Just do the one Daily Report screen. That is enough infor for now. Also trying to post multiple screen images in a post can trigger the spam filter here and your post will be delayed.
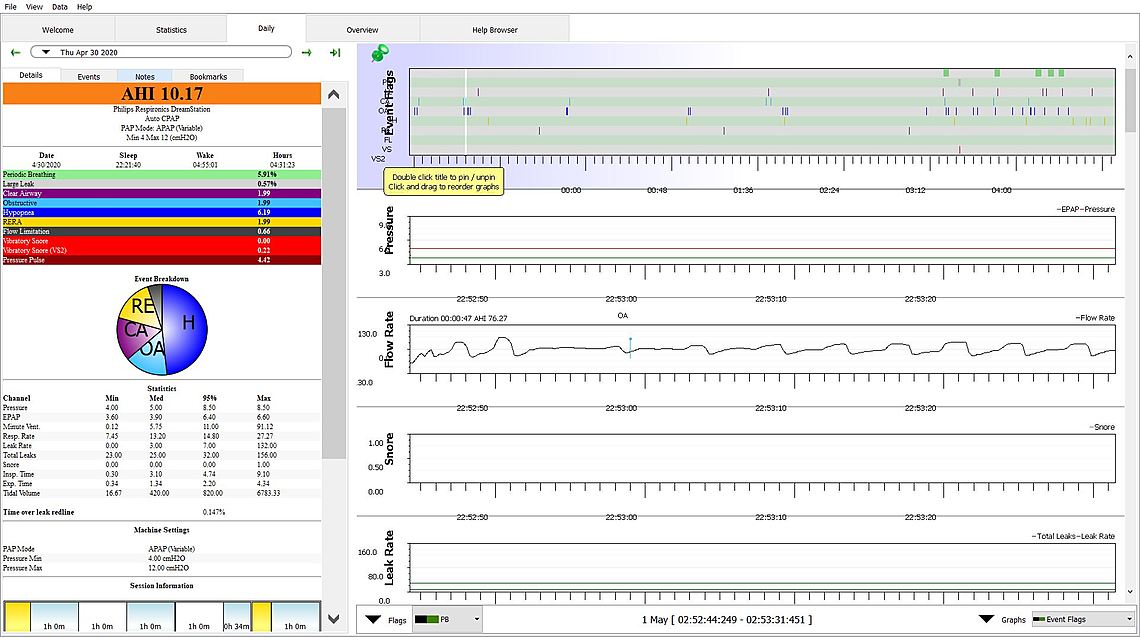
Thank you so much for your explanation, it means a lot! I believe I followed those steps properly, but am just not seeing the comment I just left where I had, from what I could see, successfully uploaded just one screenshot of my night from April 30th. I wonder if there is a delay, some filtering process to ensure that it is not spam-generated?
Yes, for new users there does seem to be a bit of a delay when images are posted. After you make a few posts it should go away. That image you posted is a bit unusual. The daily report screen shot is the most useful to post. See this thread for an example of what the screenshot should look like. The originator of that thread also has a DreamStation so the comments in that thread should be useful to you also. You do look like you have room for improvement, but until I can see the Daily Report graph I cannot suggest much. Just post one from a typical night, and hopefully it does not get delayed too long...
Thanks Sierra, I toyed around with the settings a bit so hopefully this is more valuable. I think I need to increase my pressure as a starting point, but just wondering where to start and how to progress over time based on data trends.
I use the ResMed Airfit F10 full face mask shown here (hopefully will upload).

Some tips on the layout:
You certainly do have some issues to address. However before I can comment, I need to see the full width screen for the whole night.
On the order of layout I always use the Pin function to keep the events bar at the top. Then when I scroll down to see the other graphs it always stays there so I can compare the other graphs to when the events occur. The order I put them it is:
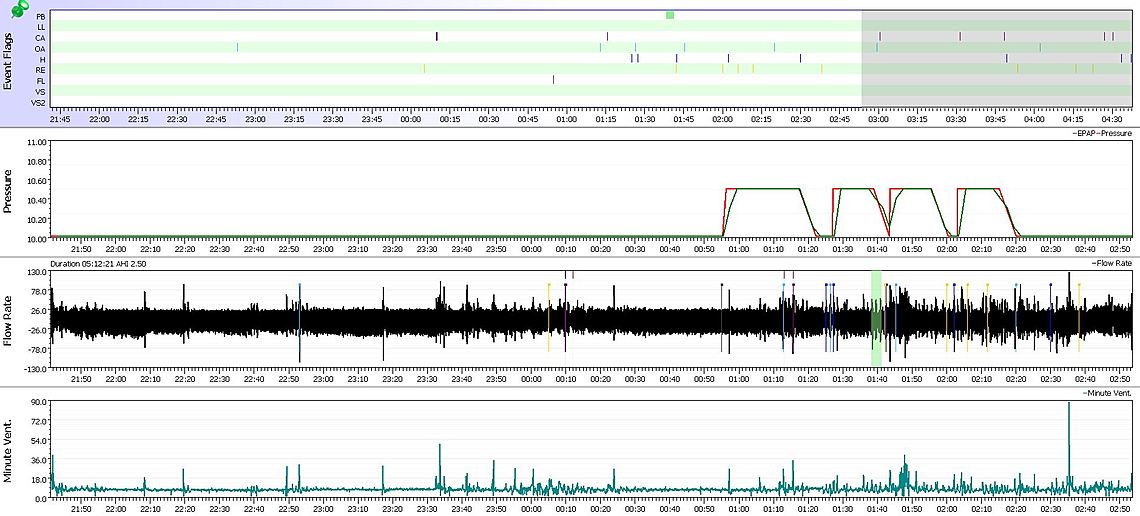
I find the minute ventilation can be helpful when looking at the issues around central apnea and periodic breathing. It is kind of a rolling average of flow rate. If it cycles up and down periodically it can cause central events.
Your results do not look unlike mine. You are having some central apnea, more hypopnea, and some obstructive apnea. As a general rule central apnea can increase as the pressure increases. The first step in trying to minimize central apnea is to minimize the pressure to the point where obstructive apnea is just controlled with the minimum possible pressure. One possible way you could reduce your pressure would be to turn off the Flex feature. The red pressure trace is the pressure on inhale and the green is on exhale. The idea is that it is easier to breath if pressure is reduced on exhale, and it does help. However, it is double edged sword. When pressure is reduced on exhale you can get OA and H events on the exhale. The green pressure is your effective pressure in preventing OA. I turn this feature off on my machine and find that I can get away with less pressure on inhale (red trace). So that would be my first suggestion. Turn off the Flex for a while and see if the red pressure line and hopefully CA events go down. With a little luck both your CA and OA events may go down just by turning off Flex. The next step if you are still seeing OA events is to increase the minimum pressure a bit more. I do see a bit of a pattern in your CA events occurring at the higher pressures (red). If that continues to be a problem after turning off Flex then I would be tempted to reduce the maximum pressure. The idea is to reduce the CA events, but not reduce pressure so much that OA events start to occur. Hypopnea events are the most difficult to figure out. I generally assume they will go down if OA events go down.
The end result of these kinds of adjustments may be that there is not a lot of range left between minimum and maximum pressure. That is not a bad thing. And at some point you might even want to consider a single fixed CPAP pressure, once you figure out what that pressure may be.
Hope that helps some. But, first I would turn off Flex and then post what you get.
Thank you so much Sierra!
I will revisit the SleepyHead application and refine my order of graphs as you have advised, good stuff!
Are there any important conclusions that could otherwise be drawn from if my machine did report mask pressure?
What is the order of concern with respect to central apnea, hypopnea, and obstructive apnea?
Do you personally, or this community in general, advocate for using a humidifier feature if available on the machine (I use only distilled water in my machine and have it set to 2/5 for intensity of humidification)?
Do you write-lock your SD card when inserting into your computer?
How to know which kind of mask, i.e., full face, or nasal, is ideal for a person?
Anything lifestyle-related or otherwise that I could implement to help me out (I noticed my apneas are lessened when I sleep on my side, but sleeping on my back is most comfortable with my full face mask, but I am always open to new ideas and trying things)?
How does one establish the cause of their sleep apnea?
Thanks, you have been enormously helpful, I will be sure to turn off the flex feature, rearrange my graphs, and report back!
I am new like you, if you are a moth breather you want a full face mask. Beyond that its trial and error. They first gave me the Dreamwear Full Face which covers your mouth and under your nose not over it. But they gave me a medium. Then I switched to a mask that went over the mouth and nose and actually fitted me with a large. That was much better but the hose comes out near your mouth as opposed to on the top of the head. Now they gave me another Dreamwear Full Face but a large and that is much better. Probably go back and forth. My insurance covered two different masks. If you only have nasal and open your mouth the air will poor out your mouth and really dry you out. I also have the philips and keep the humidity at 2, seems like anything higher and I would have to add water in the middle of the night. I consider the size of the water tray a huge problem. After 30 days I seem to finally have my mask adjusted, that has been my biggest problem, the balance between not to tight but not leaking. My pressure started at 10 and went to 18 so what worked at 10 leaked real bad when it got to 17. Now I start at 15 and max at 18 and that change really dropped by AHI. I was 89 before SPAP, averaged about 14 at 10 - 18, and now at 15-18 I am averaging around 6. But that 6 could be the supplemental oxygen they added at the same time they changed the pressure.
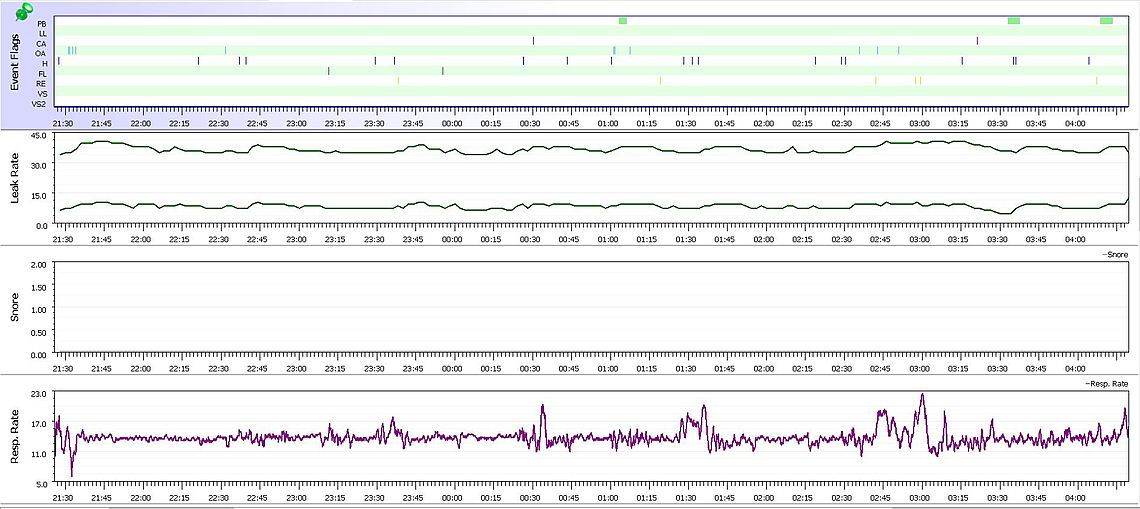
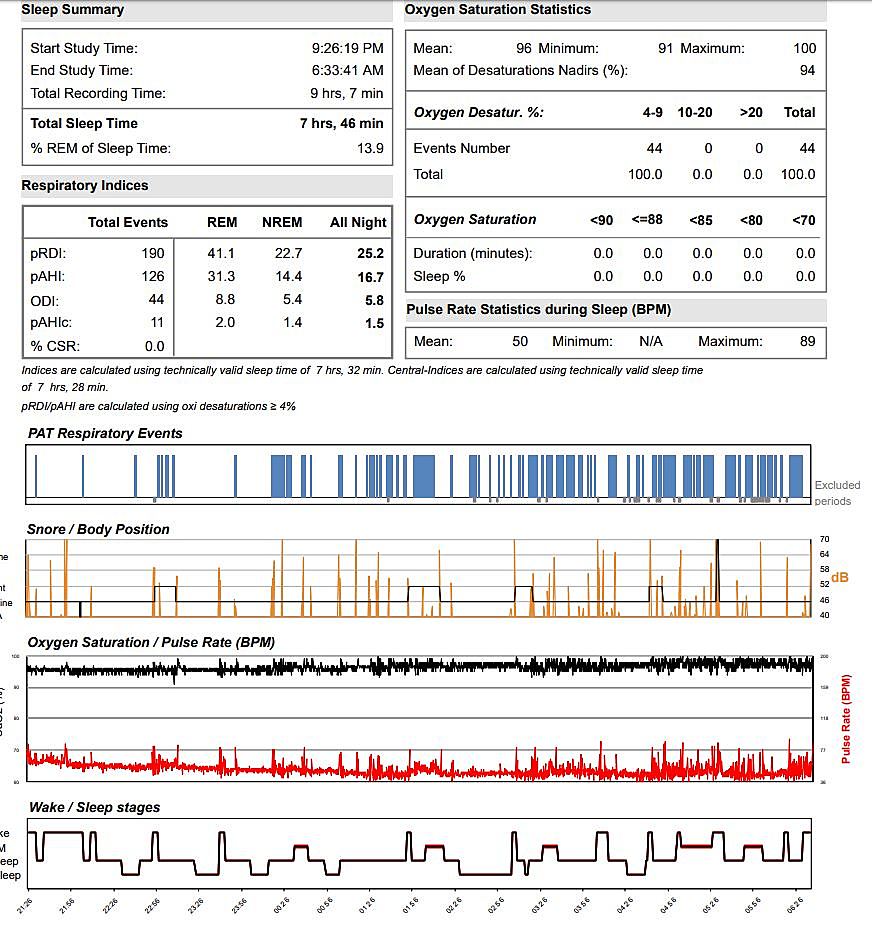
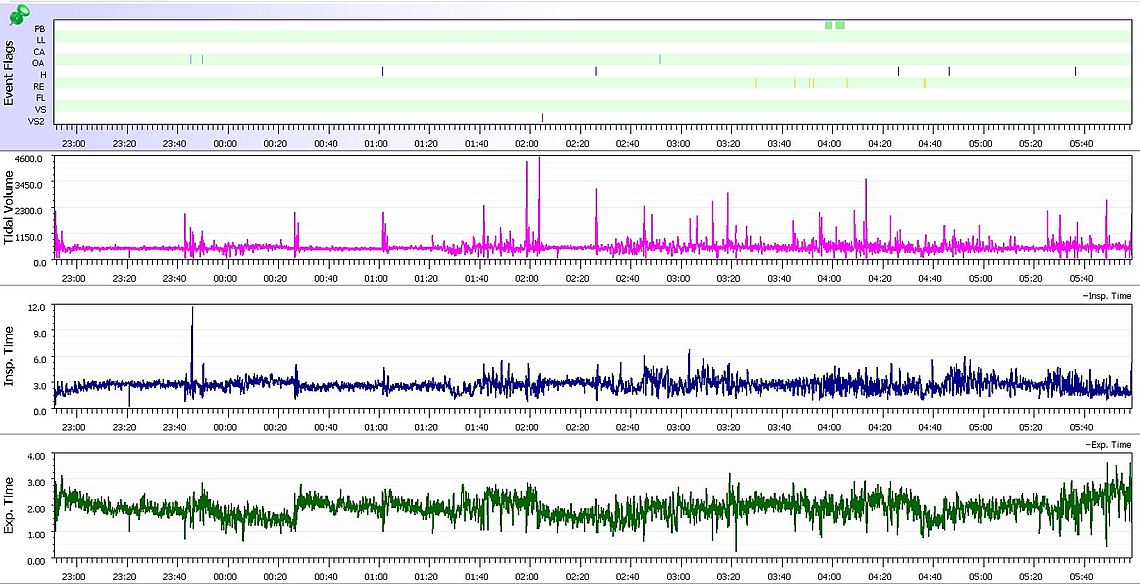
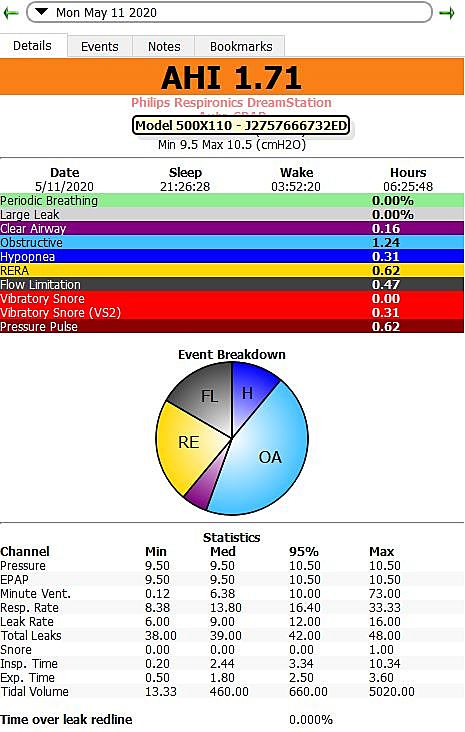
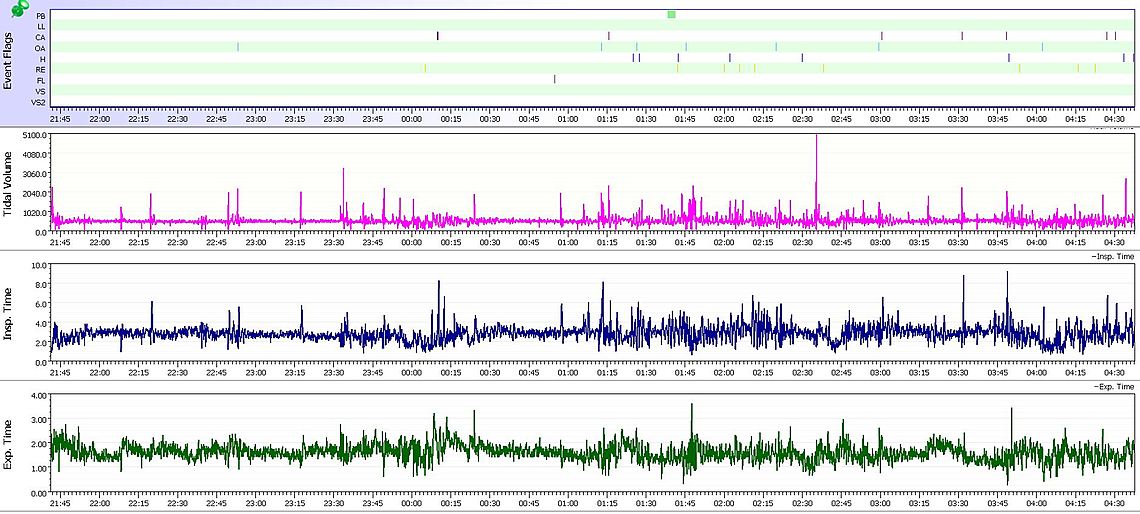
Great information, thank you both! I have uploaded screenshots of my results from last night. I made no other change but to turn off the flex (pressure was still set to minimum 8, maximum 12).
I was unable to find mask pressure or flow limitation, but otherwise have restructured my graph in the order recommended, and made it more aesthetically pleasing overall.
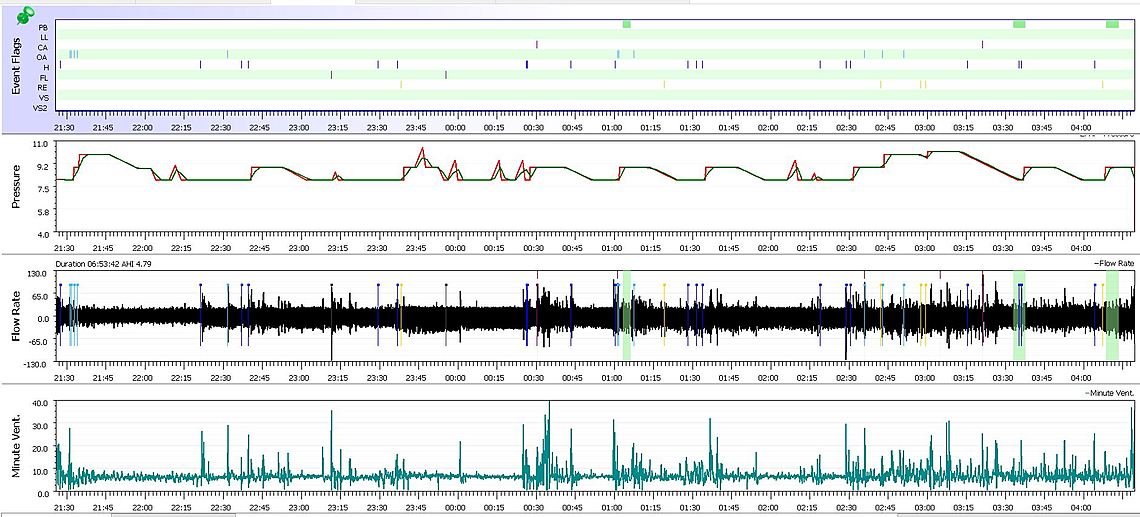
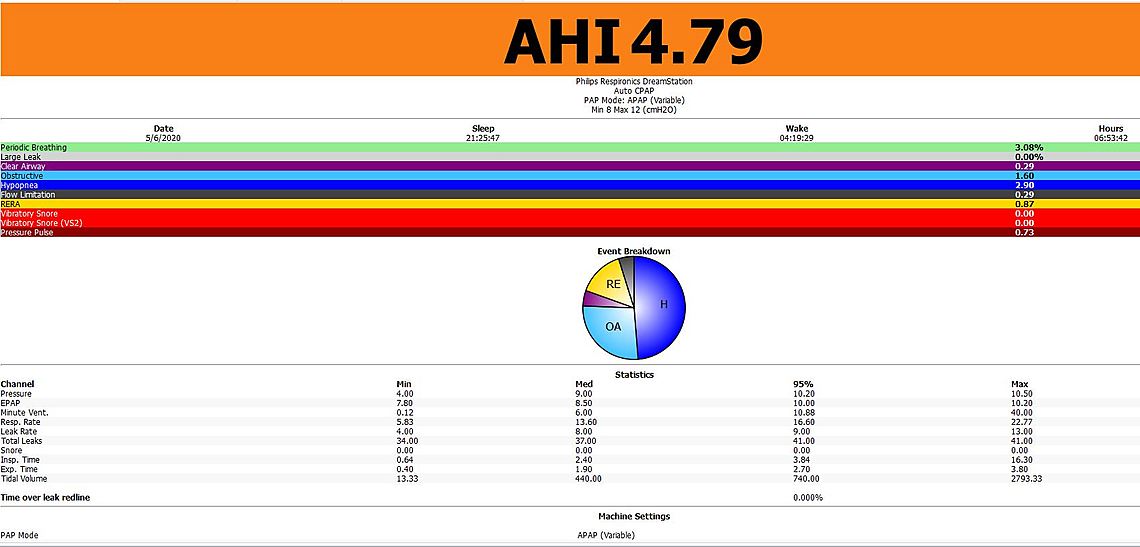
I think the good news in this report is that CA events are quite low. Most of your issues are obstructive and hypopnea. They may be solved with an increased minimum pressure. My thoughts would be to try 9 cm for a minimum and see what that does.
You do have a few green highlighted areas of what Phillips calls Periodic Breathing. They can be related to the central apnea events and a certain type of them are called Cheyne-Stokes respiration (CSR). In that other thread here about UARS I posted some examples of it. The second event you had included a hypopnea event. It would be worth looking at that more closely by repeatedly left clicking on it, or using the up down arrow to zoom in. The Minute Ventilation may be of some help in seeing what is going on there.
Perfect, I will increase the minimum pressure to 9 for tonight, and will get zoomed in screenshots of the area you suggested from last night, thank you!
When starting out with all of this I had it set to a min of 4 and max of 20, whatever the default settings were, I had no idea where to go from there, so thank you for pointing me in the proper direction!
I use the max ramp time (40 or 45 minutes I believe) starting at pressure 4 and ramping to 8, tonight will be 9. Is this advisable?
Thank you so much!
Also, to be perfectly honest with you guys, I have been shooting from the hip so to speak, and managing my sleep apnea on my own, so your input has been invaluable, and I even printed out that article on complex sleep apnea and took written notes on it yesterday, thank you so much!
I had an at home sleep study performed at the end of March (attached screenshots of my results) because for one, my Oura ring sleep tracker was detecting every night that my sleep is restless and also my sister has UARS (upper airway resistance syndrome) and I had a history of a modest degree of snoring. With the current pandemic it only made sense to independently investigate this matter, so I immediate bought the DreamStation out of pocket and seeking any and all knowledge ever since for fine tuning it, this didn't feel like something that should be prolonged. Since starting the CPAP, even though my numbers aren't the greatest, I have required an entire hour less of sleep each night and feel more rested than ever before, so it is definitely helping.
Thanks for all the guidance once again, it means a ton!
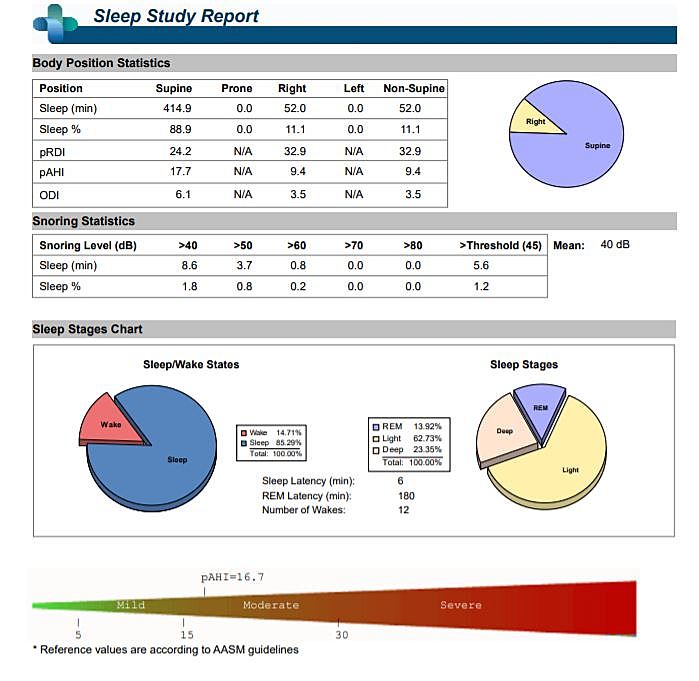
I don't see anything too unusual here. Your AHI is in the lower end of moderate apnea. No CSR was detected. If there is a weakness in this study method it would be that it does not breakdown the CA, OA, and H events. CA events are the ones you have to watch and be careful about, as they are not automatically treated with a CPAP, and may even be aggravated by pressure.
Have you ever worn a pulse oximeter overnight?
I have and never fell below 91% which was very encouraging, that was initially my concern when it had been established that I have moderate sleep apnea.
In this study they reported my result as pAHI, what exactly is that?
I have not worn a pulse oximeter and basically depend on my AHI values to indicate how well I am breathing.
I have never seen the pAHI designation before. On a quick google search it seems to be a bit of a specific brand name thing with the p standing for PAT. Not sure what the PAT designation is other than it seems to be part of the name of the machine... In any case I found this document which you might find helpful, if this was the specific machine that was used to do your test.
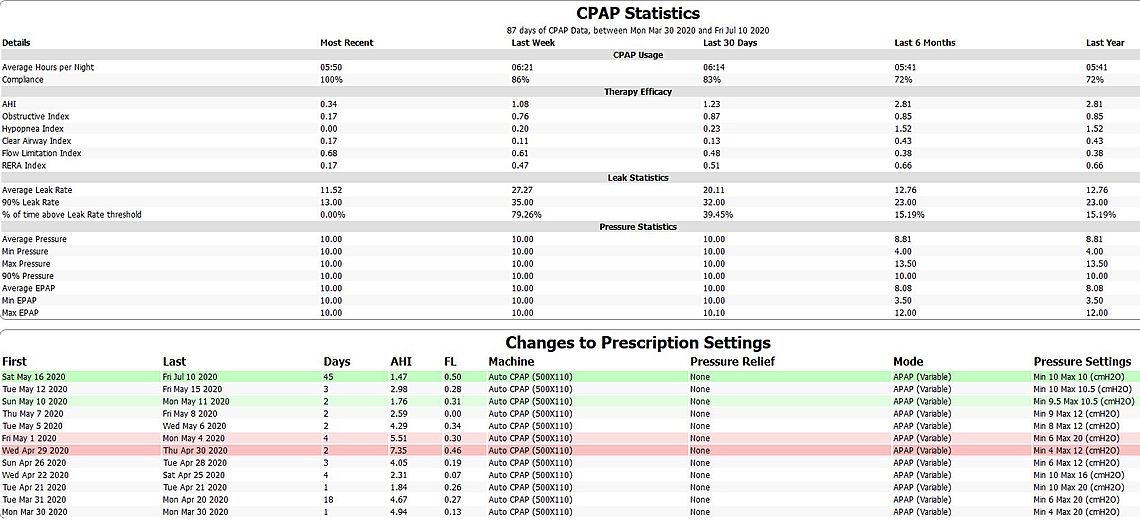
I didn't want to tell you what my daily readings are like as my apnea issues are not unlike yours, and my AHI is very variable. That unfortunately is the nature of complex apnea. My obstructive apnea is generally very good, but central apnea is a problem, and so is hypopnea. I believe a good portion of my hypopnea is not obstructive in nature, but central in nature. I have had many theories on what makes it go up and down. Part of it seems seasonal. In winter I keep our room cooler, and now that spring has arrived, the readings have gone downhill... In general my AHI has been significantly poorer since mid April. Here is a screen shot of my overview. My 280 day average AHI is about 2.5. My wife on the other hand who seldom has CA events averages about 0.8 for AHI. I was diagnosed with a home test and AHI of 37. My wife was diagnosed at an AHI of 83. It shows that where you start with apnea is not a good indicator as to what you can achieve with a CPAP.
For these reasons it is quite risky to make pressure change decisions on the basis of just one or two nights. When you get things into closer control, it would pay to wait at least a week or two between adjustments to see which setting is the best.

Both of you have come a very long way, that is very encouraging for me..
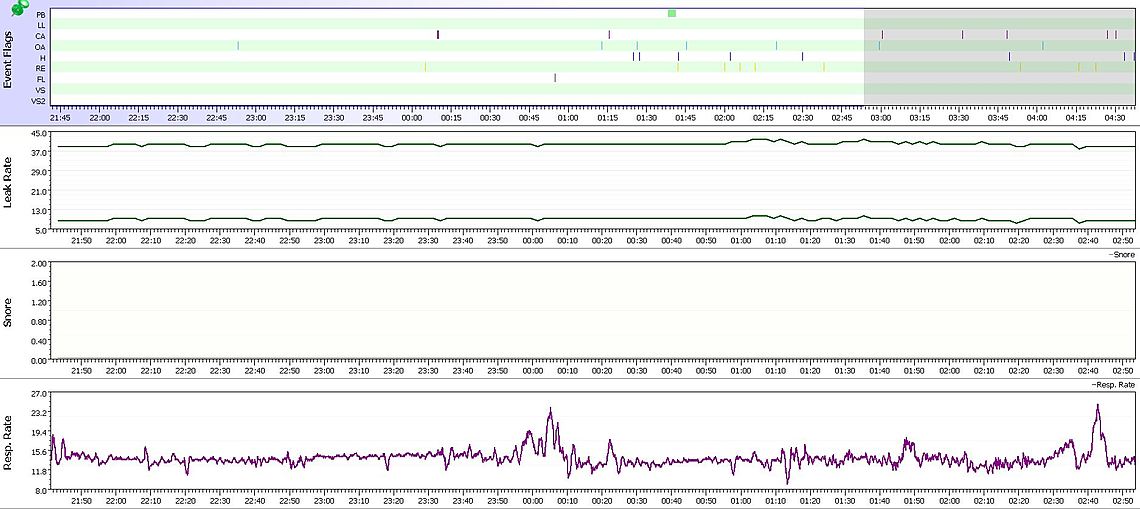
What position do you sleep in? I just noticed your leak rate being elevated at times.
I use a ChiliPad and set it to exactly 65 degrees so that in spite of every changing external conditions, my bedroom is environment is ruthlessly consistent and optimal/conducive to restorative sleep.
My best night to date! Thank you all so much for your feedback, guidance and direction. The SleepHead application said that my AHI of 1.12 was reasonably good, but this seems to be an understatement, no? I was under the impression that, with a clinical diagnostic cutoff of AHI = 5, it is "normal" for people to experience some degree of apnea/hypopnea over the course of a night of sleep. Regardless, I am very pleased with these results but always open to specific changes for improvement or for a philosophy on how to track and refine my therapy in the coming weeks, months, and years. Thank you all!
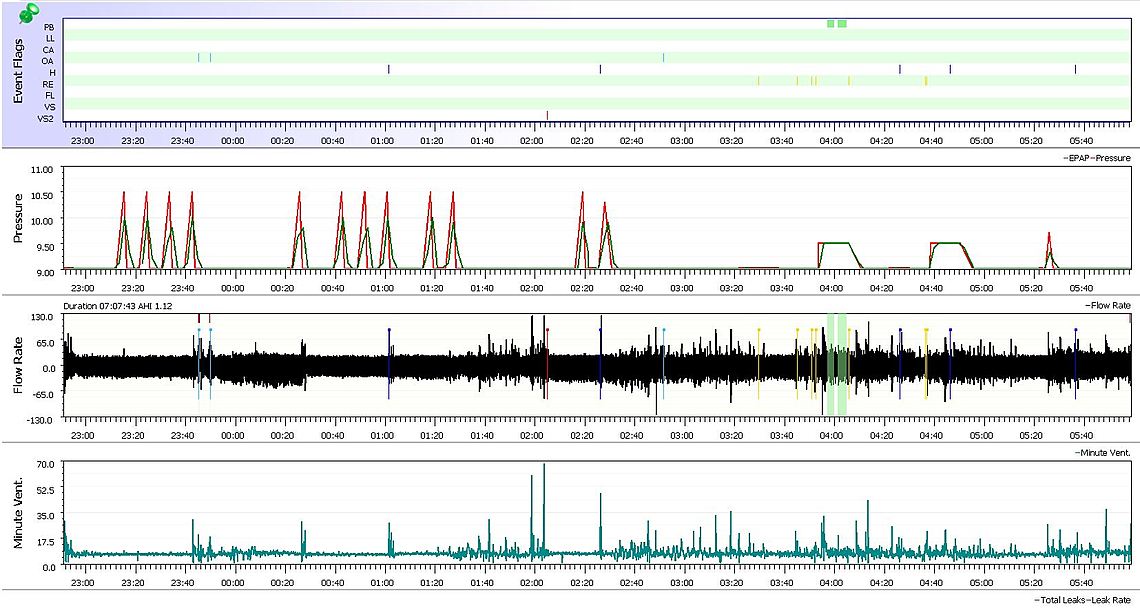
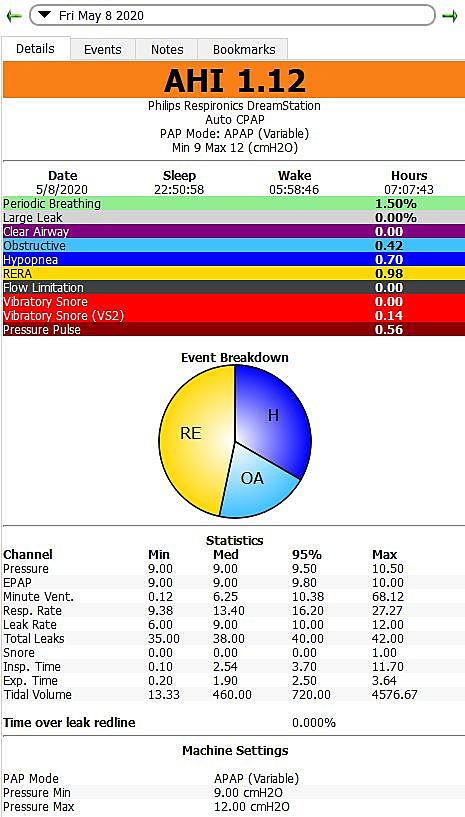
Yes, Sleepyhead can be a little, lets say harsh, with the comments. He gets really angry when you have high mask leak rates. Something like "your leak rates are horrible, see your provider immediately!". I understand the comments were removed or toned down in the OSCAR revision... One the other hand if you manage a zero events night, which I have never done, but my wife has, the pie chart turns into a happy face!
I think you are getting pretty close to an ideal setup. For now about the only suggested change I could make would be to reduce the max pressure to 10 cm. That would limit some of the pressure spiking during the night, and may make it more comfortable. In the longer term, you may want to think about trying a fixed CPAP pressure somewhere in the range of 9 cm to 9.5 cm, based on what things look like now. What is the minimum increment of pressure that you can change on a DreamStation?
The minimum incremental change is 0.5 cm.
I am considering just setting it to 10 flat, no fluctuation, and run it for a couple weeks as a baseline to draw from.
In theory wouldn't the ideal pressure be the minimum amount required to most minimize AHI without disturbing sleep comfort? I don't mind increasing the pressure if that could prevent more events. I use a 40 minute ramp time starting out at 4.
I turned off the flex feature as you advised so I'm not sure why there is both a green and red line.
Do you use the OSCAR version?
I'd be very curious to see your results with an Oura ring, even with the CPAP on a good night like last night, it detects that I am a restless sleeper which is disconcerting (highly interruptive sleep).
It looks to me that all the OA events occurred at 9 cm, and almost all of the H events were at 9 cm as well. That certainly suggests 9.5 minimum could be better. The only bit of a concerning factor is that you had two PB, or Periodic Breathing events at 9.5 cm. They can often be related to central apnea events.
I think I would try a 9.5 minimum pressure first to see if the PB or CA's become a problem. Maximum could be lowered to 10.5 or even 10. My concern in trying a flat 10 at this point is that it may cause the PB and CA to emerge. The other issue with going to a flat CPAP single pressure so early is that you do not get a chance to see what relationship there is between the pressure and the type of events you are getting. Also, a minimum of 9.5 may be enough to minimize the OA and H events.
I use the SleepyHead version. I am not sure there are any real improvements in the OSCAR version yet. I have not kept up with the revisions. There are some very minor bugs in the last SleepyHead version, but nothing critical.
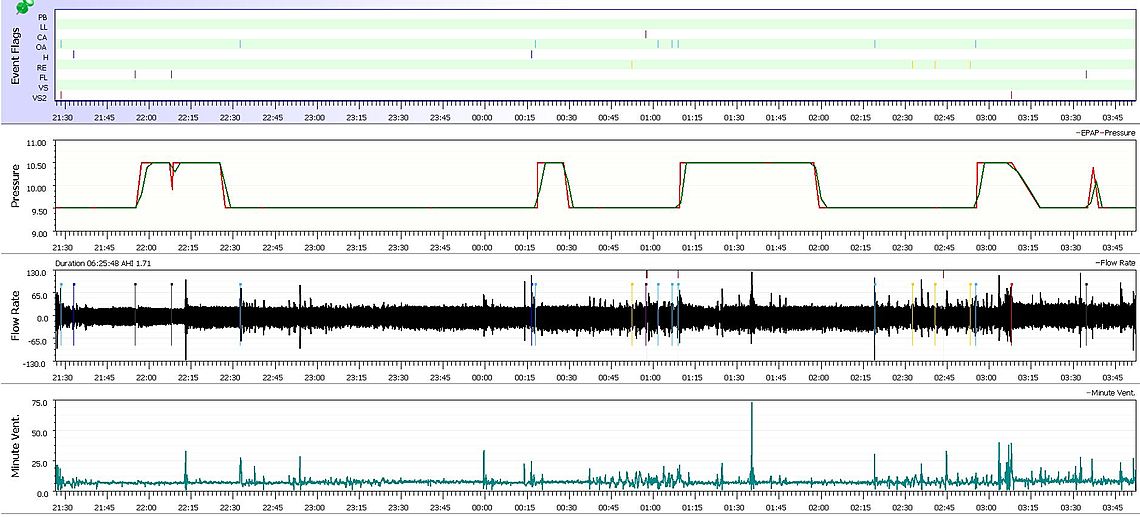
Here are my results from last night. So now I am starting to gain an appreciation for the fluctuation from night to night, but even still, I my CPAP machine has enabled me to get a much better night of sleep than ever before, and I wake up feeling rested after an hour or two less of sleep than without it which has been really interesting to note. I am in contact with the manufacturer of my advanced sleep tracker Oura ring, and going to see if I can narrow down specific times that I was in each phase of sleep (REM, light, deep) and see if there is any correlation with the specific types of events I am experiencing during those phases of sleep. That being said, even if armed with that information, I'm not sure how I would then apply that to an actionable behavior change to improve my condition. That being said, I am going to try a dental guard to decrease OA events, I will keep a journal/log of my results to find out how best to manage things.
Perfect, thank you, I will try that tonight!
What is the difference between the green and red line? I turned off flex just like you recommended.
Have you experimented with different sleep positions and seen what effect that had on your nightly report?
Any specific guidelines/advice for maintaining/sanitizing CPAP equipment (machine, mask, tubing, water reservoir)?
Thanks!
In theory the red line is the inhale pressure, and the green the exhale pressure. I think they are just estimations though. With Flex turned off they should be the same. On a ResMed they are the same. The difference may just be the accuracy of the estimations.
In general during sleep tests when they monitor sleep position more obstructive events occur when you are sleeping on your back. I suspect I sleep very little on my back, not by intention, just by the position I find myself in when I wake up.
My cleaning routine is to rinse the mask, tubing, and humidifier reservoir weekly with pure vinegar. When the vinegar is still there I add a bit of Dawn dish soap, and continue to rinse and agitate. That is followed by a thorough rinse with water until the soap is all gone. Last I hang the mask and hose up to drip dry. On the reservoir I do a final rinse with distilled or demin water.
Have been having issues posting the past couple of days. There was a privacy notice update that I had to acknowledge, but even still was having issues using Google Chrome or Microsoft Edge.
Now, only at work have I been able to construct a response (using Internet Explorer).
Thanks, I will clean my CPAP thoroughly tomorrow!
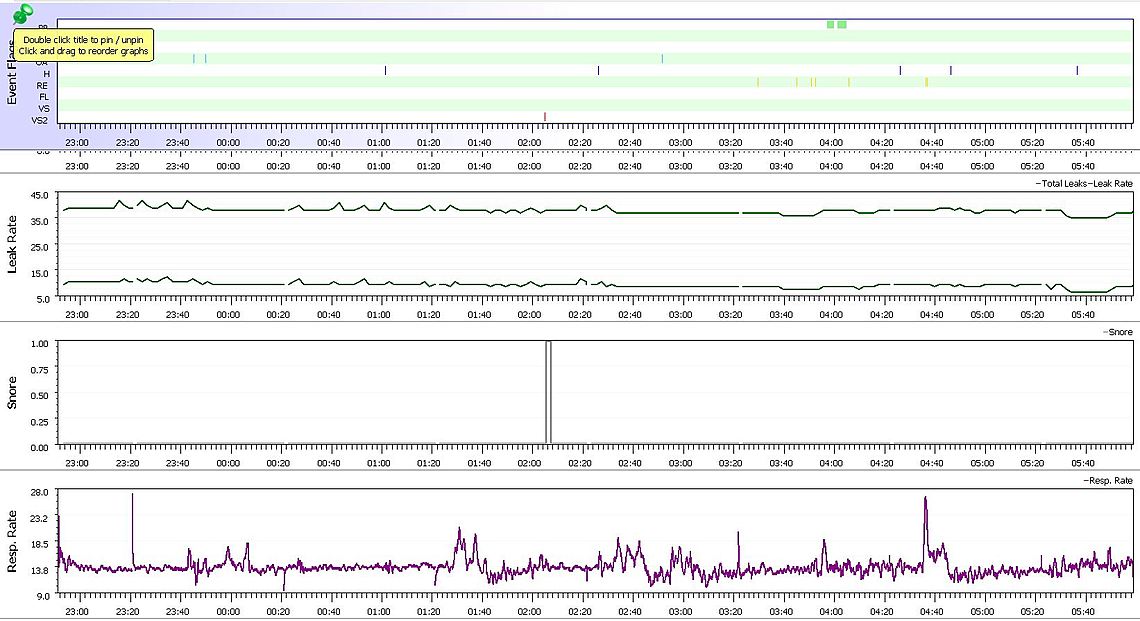
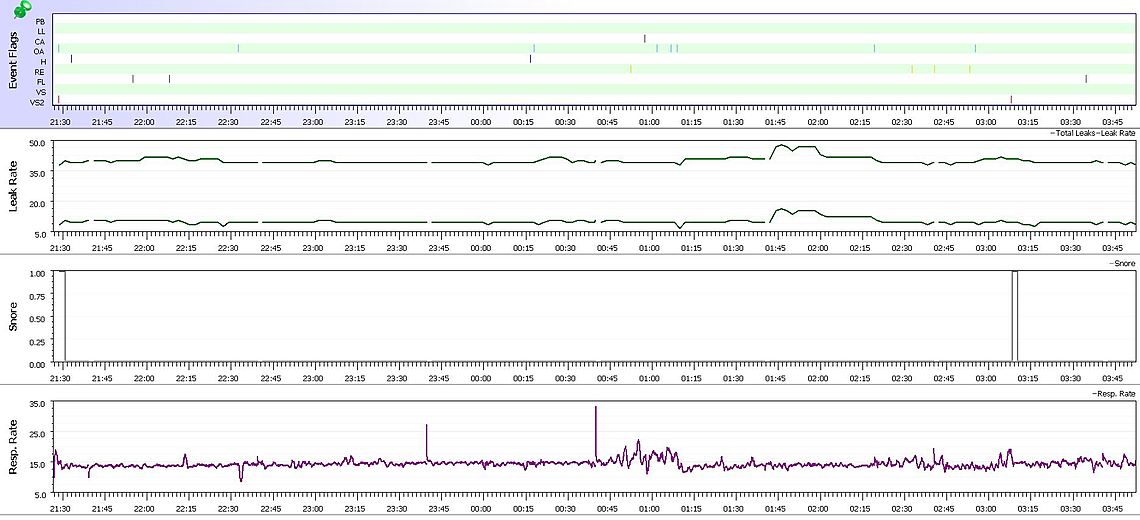
Here is the last set of statistics, min pressure of 10, max of 10.5, things got a bit worse and perhaps this speaks to your suggestion of gathering weeks of data henceforth, and then making changes bases on the trends/averages.
Would you be interested in seeing an analysis I will be doing this weekend? I have an advanced sleep tracker called the Oura ring, and I will be going through each event and seeing what stage of sleep I was in during each apnea, hypopnea, central event, etc. I am trying to collect as much intel as possible :)
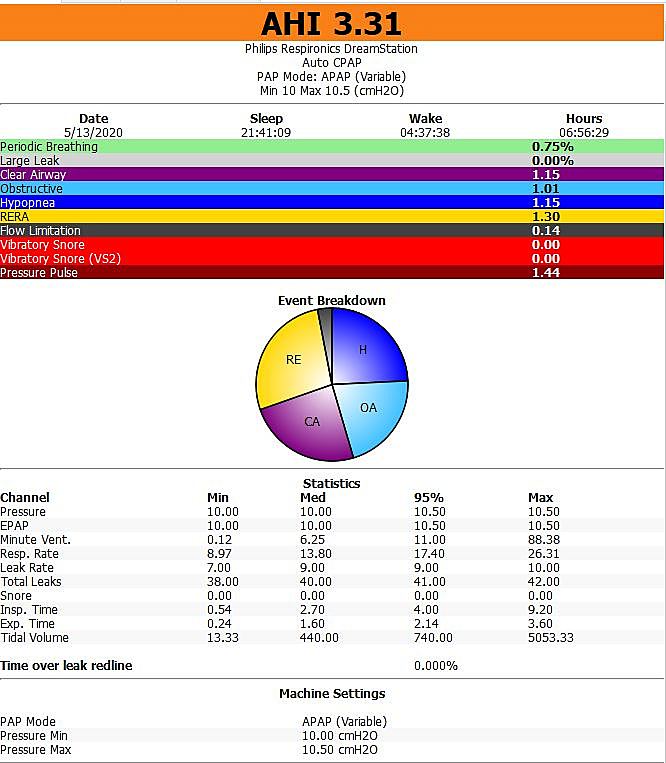
About all I can say is that your event types are relatively balanced, and you are probably close to an optimum pressure. You are partly zoomed in so it is hard to match up the events to pressures. What you might want to think about is to pick a pressure and switch to CPAP mode for a week at each pressure. It is one option to try. From what I can see, I may suggest trying 10 cm first.
On your Oura ring, I don't know much about it. Would be interested in seeing the results though.
I use Google Chrome and have at times noticed some glitches. Sometimes I try to open a thread that has multiple posts, but when I open it, there are no posts.
I haven't uploaded to Sleepyhead in months, currently trying to figure out how I generated those graphs initially. But needless to say, things are going extremely well for me at 10 cm.
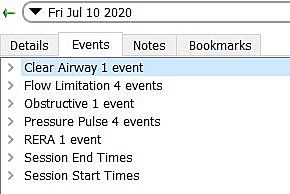
I'm just not understanding what my machine considers a clear airway event vs. flow limitation vs. obstructive vs. pressure pulse vs. a RERA event.
"I'm just not understanding what my machine considers a clear airway event vs. flow limitation vs. obstructive vs. pressure pulse vs. a RERA event."
A clear airway event is when there is no obstruction of flow. You just don't breathe in or out. Clear airway events are essentially central apnea events. Flow limitation is when the machine senses restriction in flow but not enough to cause an obstructive apnea event or hypopnea. I am not a medical professional but here is my understanding of the types of events, in order of severity:
Both CA and OA events are not good. CA is much harder to treat. Flow limitation I am not so sure about, but it may be a partial hypopnea that does not go to 10 seconds in duration.