I have come across other references to people developing edema after starting CPAP. I just started CPAP the beginning of April and I was loving it (Airsense 10 For Her). My pressure averages just over 6 and with that my AHI went from 45 to less than 1. I am tall and thin and have joint hyper mobility, but do not fit the definition of full blown Ehlers Danlos Syndrome. I suspect that my loose connective tissue is what gives me sleep apnea as my soft palate falls back very easily. That would also explain why such a low pressure works for me. Anyway, in midMay I woke up to find both legs quite swollen (pitting edema), something I had never experienced before. I had been having trouble with my nasal cushion fitting properly that night and when I glanced at the pressure during the night it was between 10 and 11, something I had never seen before. A curious thing about the edema is that it got better during the day. Usually you would expect leg edema to get worse during the day because of the legs being “downhill” from the heart. I struggled with mask fit again the next night and the edema continued (not sure of the pressures the 2nd night). I then got a new nasal cushion, had a good fit, pressures seemed to stay low and my leg swelling went away over the next 2 days and has not returned. I have also turned off EPR and gradually lowered my maximum allowed pressure (it is currently set to 7.) My AHI was 0.3 last night so I feel comfortable with that but will continue to monitor.
I have not been able to find any info on the web about this other than people who posted here a couple years ago with similar stories, except that their swelling started right away with CPAP. My best theory is that because I have very loose connective tissue, the increased intrathoracic pressure when the CPAP pressure went up led to decreased filling of the right atrium and therefore a backup of fluid most noticeable in the legs.
I did have a normal echocardiogram in January and have no heart disease. The swelling did not cause any breathing problems either. I would love to hear from anyone with similar experiences.
First off, to be clear I am not a doctor. I have used CPAP for a couple of years and my wife longer. I can't think of any direct way leg edema could be caused by the CPAP. I would be looking other potential causes like a blood pressure medication such as amlodapine. A water pill like indapamide may be a better alternative. There are a few other drugs which may cause it like Actos and Avandia for diabetes. Congestive heart failure can also cause it.
Have you used OSCAR to look at your AirSense results in more detail? It may offer some clues as to what may be going on. Low blood circulation can cause central apnea. If you are having central apnea events that may be a potential cause.
I actually am a doctor myself and it does make sense that a high enough pressure inside the chest cavity can restrict blood flow return to the right atrium. The question is how high a pressure is needed to do this? In most people it is obviously much higher than the usual CPAP pressures. In my case I am speculating that because of my weak connective tissue my vena cava partially collapses more easily, thus restricting blood return. I agree that the meds you mentioned can cause leg edema, but the only medication I am on is low dose beta blocker for sinus tachycardia. Not to mention the fact that the swelling has resolved completely and not returned since I have kept the pressure below 8. My most recent results showed 0.2 AHI, 0.1 central. I am getting the data from the clinical menu, I’m not familiar with OSCAR but will check into it. Thanks!
As you will know 8 cm of pressure is pretty low. A CPAP goes up to 20 cm, and a BiPAP which many use will go up to 25 cm of pressure. I now run my AirSense 10 on a fixed pressure of 11, with it set to use 9 cm during the AutoRamp period. I find the pressure refreshing, and anything less than 9 while I am awake kind of suffocating. I don't like to feel short of air when I take a quick deep breath. I am amazed that some people can tolerate a 4 cm pressure to start the ramp.
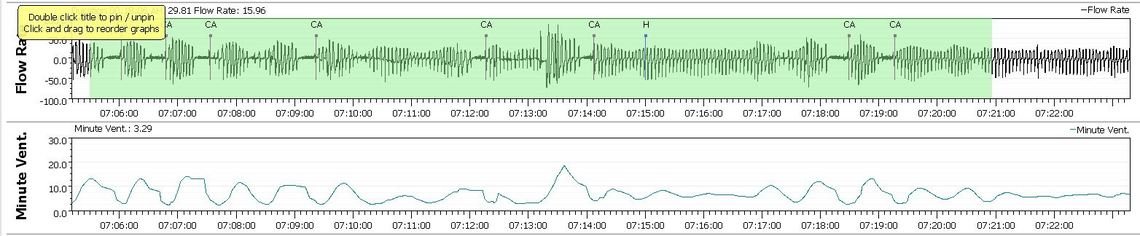
I have issues with central apnea and have blamed the bisoprolol beta blocker for some of it. I was taking 5 mg a day and felt it was slowing my heart and blood circulation too much, and the oxygen/CO2 balance which controls the reparatory rate was unstable. This in turn I believe was causing the period breathing or Cheyne–Stokes pattern, and central apnea events. I reduced my dose to 2.5 mg a day as a test and I believe my central apnea frequency improved quite a bit. I showed my doctor the results and he agreed with the dose change as my blood pressure was still very good, but I think was kind of skeptical of me blaming the beta blocker for causing the central apnea. With OSCAR you can see all of this data displayed graphically, and can zoom in on the detail. There is a condition called treatment emergent complex sleep apnea where someone new to a CPAP experiences high levels of central apnea when first using the machine. In most it goes away after a few weeks. For me it did not. I believe the underlying cause is that the CPAP upsets the control system stability. The solution is to keep the pressure as low as possible but still control the obstructive apnea. Here is clip from the graph that shows what it looks like in OSCAR.
So in some situations CPAP pressure can be an issue. I am just not sure how to connect it to edema though.
One of the things you may want to try is setting the machine into CPAP mode and going to a fixed pressure. That way you take control away from the machine and not let it increase pressure too much. In my case when I had it in auto mode it was responding to hypopnea events with more pressure while the hypopnea events were actually incomplete central apnea events. Then more pressure makes the central apnea worse instead of better. That is why I went to a fixed pressure. It did a good job of reducing AHI and in particular central apnea. However it did not improve hypopnea. More recently I have turned EPR back on with it set at 2 cm. That has virtually eliminated my hypopnea events. Not sure how and why, but I have a little suspicion that EPR is doing enough to prevent the machine from flagging events, but not really changing my breathing much at all. Numbers improved, but perhaps outcomes not so much. It is nice to see lower numbers though!
Hi, I hope you are still here. I have a theory as to why I at least, get edema - my albunum was a little low, I am 70, had no edema until I started the machine. I used to get up 2 - 3 times a night to pee and made a beeline for the bathroom in the morning. The change is not because I am sleeping away - I still only sleep 3 - 4 hours on a good night. I have a Pituitary tumor which then causes problems to hypothalamus, pineal gland etc. I drink a good 2 liters of fluid a day, with a lot at night, the later in the day the thirstier I am. Now I take 2 furosemides in the morning and am on blood pressure meds too, my pressure was always normal prior to the machine.
So if at my age I have most likely thinning/weaker veins, capillaries that might be leaking and then you add air pressure to this mix could this make your veins and capillaries leak more fluid into your body? I realize the amount of water in the take is not enough to cause edema - but I had decent urine outflow and now I don't after using the machine - some mornings after not going all night, I pee out a whopping couple of tablespoons.
And of course I have mentioned my theory to five docs now and gotten downright absolutely NOTs, to Impossible to be laughed at - and told no one has this happening - well a LOT of people on just this forum have this happening.
Is my Theory any good?
I'm hoping that you've found some information since your original post... I'm new to my CPAP (AirSense 11). AHI was 70 (!!), with a mix of (mostly) OSA and CSA, down to less than 2. I've been using it since 2/14 and, other than obesity, have no chronic issues and take no medications. I've only ever experienced LE edema sporadically during long distance car travel (10-12 hours). Currently, I have my settings at: auto ramp at 4 and it runs up to 11 overnight. I use nasal pillows with zero leaks and have had no adverse issues until this started over the last week. This was the only information I've found regarding increased LE edema with CPAP use!
There have been many discussions on the apparent link between CPAP and Edema, but for us mere mortals it seems way too complex to really get a grasp of.
Inevitably they must be connected, but then everything that impacts on the body is connected to everything else via one mechanism or another.
Just being human and ageing would link everything even if it is through numerous interactive systems.
In many ways sleep disorders are central to, and perhaps even pivotal to, a wide range of other disorders.
From a different perspective, even considering that there might be a link forms a link and certainly acting on those beliefs creates direct links and quantifiable effects.
The question isn't: "Are they connected?" but "How are they connected?" and "How do we co-ordinate the treatments?"
Something else to ponder at 4am.
:P
Just wanted to leave an update re: leg edema developing overnight and resolving during the day after starting CPAP and pressures went higher. I eventually settled on putting my machine in CPAP mode with a pressure of 4.5 and remarkably that has given me great control of my apnea with (AHI) almost always less than 1. I have had absolutely no recurrence of the nighttime leg edema since keeping the pressures low. I do have a little daytime edema from bad veins, but this, as expected, gets better overnight.
I know I still have apnea to treat because only when I occasionally take off the CPAP in the middle of the night, my Fitbit shows a spike in my oxygen variability.
Obviously most people tolerate and need much higher pressures than this, so I can only assume there is something different in how I am “put together”. I talked about this in my original post. I suppose if I really wanted an answer I could let the machine go back to a higher pressure and see what happens but I find that prospect a little frightening and have decided to leave well enough alone.
And as a note to those of you who have reasonably suggested other causes of leg edema (eg medications or heart failure): in these situations the edema is always worst at the end of the day and best in the morning as having the legs elevated helps them “drain”. My situation was the exact opposite.
I am a dentist working in dental sleep medicine. Have you considered switching to an oral sleep apnea appliance. There is zero pressure required. You could also consider wearing an oral appliance WITH your CPAP. That would lower the required pressure even more. Dr. Arthur B. Luisi,Jr., The Naples Center For Dental Sleep Medicine.
Thanks for the suggestion, but I already have my pressure set as low as it will go so not much to be gained there. I have also over the last year or two developed an enlarged tongue which definitely reduces my oral airway and it’s hard to imagine any tolerable oral device could counter that. I have had a thorough medical work up, including biopsies, with no explanation for the enlarged tongue(I’m not overweight either). Looking back, this tongue enlargement may be the cause of my sleep apnea. It now protrudes over my lower incisors and pushes up against my upper incisors. It overlaps my molars. It has shifted my bite. With my nasal CPAP on I no longer even have to sleep with my mouth closed as my tongue easily seals off the back of my airway when breathing through my nose. I’m a little worried as to what will happen if my nose is blocked from a cold.