There is a condition known as emergent central sleep apnea that affects about 10% of those undergoing new treatment for apnea with a CPAP. In about 75% of these cases the CSA goes away or is reduced to acceptable levels in about 2 months. In the other 25% it remains a problem. These numbers vary depending on the study, but these ones are in the ball park. So perhaps in 75% of the cases the brain does retrain itself to control breathing better as is suggested in your article. Here is a link to one of the articles on the subject.
Emergent central sleep apnea during CPAP therapy-clinical implications
I was one of the ones in the 25% where emergent CSA did not reduce after 2 months. However after 9 months now, things are starting to get better. Yes, it could be the brain being retrained finally, but I think it is more due to a change on my part to a fixed pressure CPAP mode for machine setup. I think my machine was chasing hypopnea events with more pressure, and the higher pressure was causing central apnea events. The problem with the machine is that it cannot tell the difference between a hypopnea event that is obstructive in nature or central in nature. If it chases central hypopnea with more pressure it just makes things worse. At least that is my theory, and the results I am getting seem to verify it. I was running pressures as high as 15 cm in auto mode, but now I am using a fixed pressure of 11 cm and getting much better results.
Hope that helps some. If you can post more detail on your issues I could give you my thoughts. I find SleepyHead to be invaluable in figuring out what is really going on.
Hi obbyone.
I haven't had any experience in this field.
Someone was here a few days back discussing breathing and throat exercises which I guess may be involved in your subject.
Your link seemed quite interesting till I got to the last paragraph. :O
I could never really understand the various medical fields that consider reverse provocation to be a safe method.
Or did I totally misunderstand the intent?
Central sleep apnea is difficult to deal with, and there is no simple, one size fits all solution. It depends on underlying causes. One of the better articles I have found on the subject is at this site. See link below.
Previously I started on a CPAP in April 2016, I had my first Sleep Study and got 39 AHI... I was diagnosed with OSA, I used the CPAP for about 2 years with lower AHIs results until the second year where my AHIs went terribly higher...I was feeling fatal even with the CPAP, blood pressure came back even worst (200/110) and experienced premature ventricular contractions for which I had to be admitted to the hospital on Jan 12th, 2018 , I thought that I was having a heart attack! Thanks God it wasn't one, but my life changed since then. I went thru 2 more sleep studies and I was diagnosed with Central Sleep Apnea (I honestly think the CPAP caused me that...) Now my pulmonologist says i no longer need the turbonoplasty to correct my septum since my problem has become a problem with my neurons and brain. I have been with my BiPAP machine for three months where my AHIs have been >3 & <5 but I have realized just recently for the last two days that my numbers have reduced considerably to < 1 AHIs. Currently my Resmed Aircurve 10 ST is set to EPAP 14 IPAP 20 START EPAP 6 and ramp time 45 min. Only complain at this point: Aerophagia and too gassy. Today my blood pressure is normal, memory issues and anxiery/panic attacks are gone too.
I have been looking for alternatives and have found internal and external "pacemakers" to stimulate the diafragm and lungs
Respicardia http://www.respicardia.com/remede-system
Inspire https://www.inspiresleep.com/what-is-inspire-therapy/how-inspire-therapy-works/
Avery Biomedical http://www.averybiomedical.com/success-stories/central-sleep-apnea/ut
All these methods need mostly invasive surgeries with a bunch of risks which I was considering until I found the unknown "neuroplasticity". My doc laughed about it when I mentioned neuroplasticity to him...i guess our business is over if I get cured with natural methods if any. 😁
Thanks for reading.
Some comments on your situation:
The normal progression of CPAP treatment when CSA becomes a problem is to move from an APAP machine to a BiPAP, and if that fails to an ASV. I recall that there are studies which have shown that the move from APAP to BiPAP in about 60% of the cases caused CSA to get worse, not better. I think the treatment path is largely driven by insurance company rules. Start with the cheapest machine and move up when they fail.
Your ST machine is kind of crude ASV where it is trying to help you breathe and has a backup trigger when your are not making a good effort to breathe. The ASV takes that one step further and locks on to your actual breathing rate and assists you breath by breath to keep breathing. Making the ST type work can involve a lot of trial and error to get the settings right.
I think there can be an opportunity that slips through the cracks in treating CSA, and it is the most basic -- fixed pressure CPAP but at a low pressure. Some people can be very sensitive to pressure and a CPAP using too much pressure can cause more problems than it solves. That is the direction I have gone with some success. I use a low (relative to where I was in Auto mode) fixed pressure with no EPR, so IPAP=EPAP. It seems to be working. My biggest contribution to AHI now seems to be hypopnea events, which I suspect are central in nature.
Have you used SleepyHead to examine your flow date in close up detail? A lot can be learned by examining the flow, mask pressure, and minute ventilation relative to when events are occurring. You can also see if Cheyne Stokes respiration or periodic breathing are a problem.
Could there be any medications which could be contributing to the issue? I have convinced my doctor to cut my dose of a beta blocker for blood pressure in half. These drugs tend to slow the heart rate and I suspect potentially contribute to CSA as a result of lower blood circulation rate.
I used sleepyhead a few months ago, but I think my SD card got messed up. It can not be read any longer.
By the other hand, I recently got sick during Xmas with strep throat and I have been taking a very strong antibiotic (cephalexin)...in the last 4 or 5 days my AHIs have been increasing (4>AHIs<7.5). Is this because of this treatment or could be my coughing being detected as apneas? What about ocassions where I burp little by little due to the aerophagia?...I also have to expel bunch of phlegms at this time.
My biggest fear is to get sick with pneumonia, bronchitis or flu while having this sleep apnea issue. I always clean my equipment in a proper way.
I am worried now...
On your SD card, make sure the lock switch is off when it is in your machine. If that does not work, you could reformat your SD card with a computer, and then put it back in your machine. The machine should then automatically set up the card properly. Last resort get a new SD card.
Zooming in to the detail in SleepyHead can let you manually decide if events are real or not.
It is worthwhile to do a weekly clean of your mask and hose. I uses pure kitchen vinegar first, followed by water and dish detergent, an finally a rinse with water and hang up to dry. Pure vinegar is strong enough to kill any bacteria.
On the flu and pneumonia I would make sure to get your flu shots annually, and also get the pneumococcal vaccines. For the best coverage there are two of them. One is the standard pneumococcal and the other is Prevnar 13 which extends the protection more. People do not often die from the flu, but one can die from pneumonia which develops from the flu.
Thanks for the advise. I did switch off the lock on my card before running sleepy head. Like i said it only worked once.
Thanks again.
If your data is all trashed, you may want to make a clean start by uninstalling SleepyHead, do a download of the current version, and install it. Create a new user account. Reformat the SD card and put it in your machine. It should tell you that it is setting up the card, and I would expect give you an error message if it can't use the card. After you use the machine then take the SD card and try importing the data.
A BiPAP ST is not a crude ASV. They are 2 different (although related) devices with 2 different purposes. Putting it simply, BiPAP ST (and other similar modes of BiPAP) are used to help someone breathe more, increasing their oxygen levels and decreasing their CO2. However, if your CO2 is not elevated this can send it too low and induce or exacerbate Cheyne Stokes Respiration. This is where ASV comes in. ASV is used to even out respiration without increasing ventilation, thus removing central events without causing problems due to CO2 levels being too low. BiPAP ST helps someone breathe more but ASV helps them breathe more evenly without making them breathe more. It is more complicated than that in reality, but that is the gist, and treatment is (or should be) tailored to the patient's needs.
Thanks for the explanation. My cursory review of the technology (which may be in my future for treatment) is that the AirCurve BiLevel machines monitor breathing on a more macro basis. They see breathing depth and rate going down so they boost pressure support somewhat blindly to try and prevent it. Depending on the model they may have some adjustments to control the switch from EPAP to IPAP to improve the breathing support effect. And also depending on the model they may have a fixed backup rate at which they will provide pressure support somewhat blindly trying to maintain breathing at a fixed rate when the user is not trying to breath. The ASV model on the other hand looks at Minute Ventilation and breath by breath flow. When it sees Minute Ventilation falling it responds on a breath by breath basis by boosting pressure support but in sync with any breathing effort the user may still have. In theory Minute Ventilation will be maintained as constant as possible. That was my conclusion. I like to simplify technology to an understandable level. My conclusion was that the basic BiPAPs were doing in a crude manner what the ASV does in a much more sophisticated manner on a breath by breath basis. Yes, it may be a bit of an oversimplification.
I think the sad part in this, and my current opinion for my own future, is that a BiLevel machine is not all that useful. It is more likely to create more problems than it solves. My thinking now is that I will use a basic CPAP for as long as I can and then go straight to an ASV if I can't control central apnea any other way.
Hi all, I was able to export my stats by using a different SD card and sleepyhead software. My numbers look different from what the Resmed Aircurve 10 machine provides, is this correct? (In the machine are actually a little bit worst)... Hope someone expert can see my screenshot stats and let me know if I am doing ok... last night I had a big leak by using my nasal mask (I usually use a full mask, but I used the nasal once in a while to see if it works)... I opened my mouth very probably. Thanks
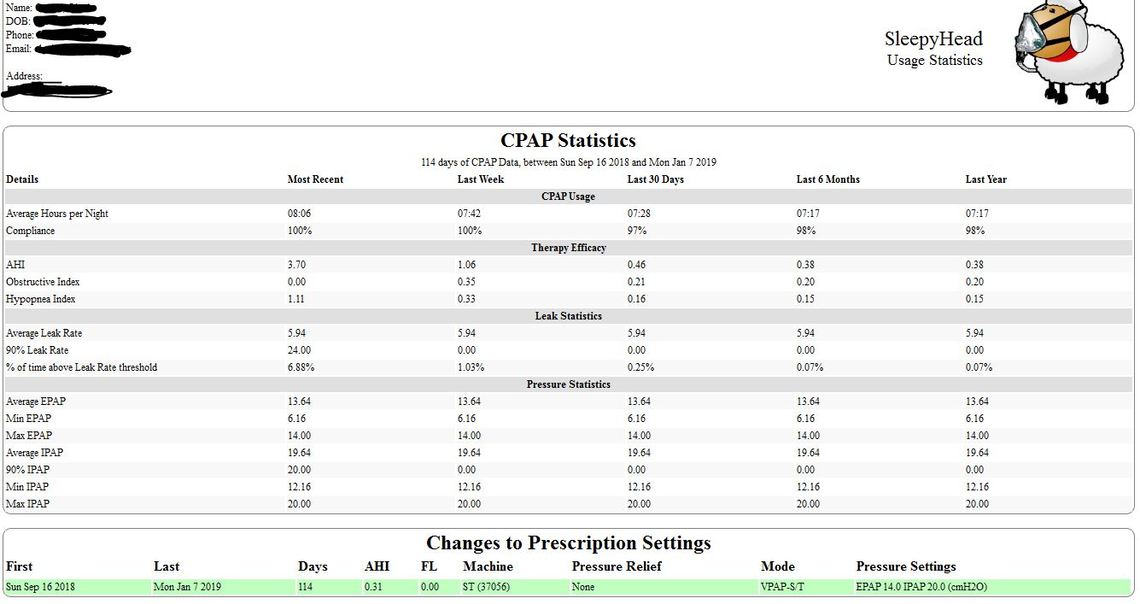
Based on your numbers I think the SD card has not been in the machine or was not working except for the last night. Certain summary data is kept in the machine memory and you appear to have that for some time. That would include the CPAP Usage numbers, and the Therapy Efficacy numbers. Your AHI for Jan 7 was a bit high, but your averages for longer periods look good, providing they are valid. I think there may be a bit of a setup issue in SleeyHead as it is not showing all categories of Apnea events like Clear Airway events. Your Obstructive + Hypopnea events do not add up to the reported AHI number, so something is amiss.
Your Leak Statistics and Pressure Statistics look to be one night only - Jan 7. This makes me think the SD card was missing or bad. There is no real way to recover that, unless you had good data in SleepyHead before you had SD card issues? If you did have good data before let me know and there may be a way...
Your one night leak data was not all that bad. I have seen much worse. The Daily Detail page would show much more. Mouth leaks tend to be isolated with flat tops somewhere above 25 l/min.
If you can post the daily detail page it would be much more helpful in determining how you are doing. If you want to exclude personal details one way is to go into SleepyHead and use File, Edit Profile, and page through the screens using the Next button, and delete those personal details. You cannot change your User Name once you have set up that Profile. The only way is to create a new Profile with a less descriptive first name or nickname. You can probably do that without losing much data. What you have is on your card, so when you create a new profile it will be transferred from your card into the new profile.
If you are using Windows 10, another option is to use the included Snipping Tool. I find it very handy to capture sections of a screenshot (to exclude personal details for example).
Thank you so much Sierra... So overall my numbers are looking good? Why Resmed app online shows different numbers? I will upload the Resmed screenshot in a bit...
The ResMed on line (MyAir?) is to my knowledge only reporting the summary data not the detailed data. And you seem to have lost your detailed data except for one night. You should be good going forward now that the SD card seems to be working. Which numbers are you seeing as different? The other possible issue is that SleepyHead does have some bugs which vary depending on the machine used. Your machine type may have some particular bugs in the SleepyHead software. I don't understand why only AHI, OA, and H events are being reported. If you post the Daily Detail screen I may be able to figure out more.
These are my daily stats shown by sleepyhead
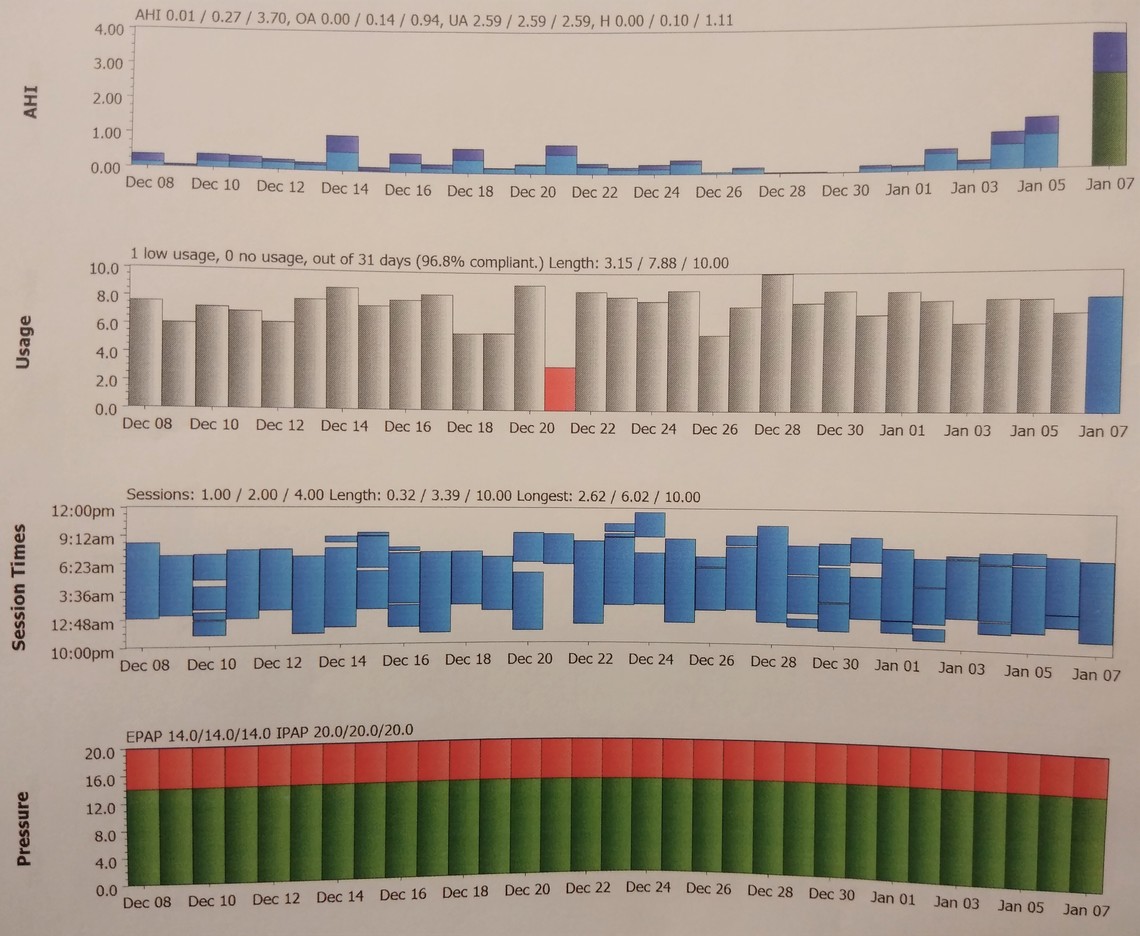
As you can see...Sleepyhead shows less than 2 AHIs for Jan 1st thru Jan 5th, but the Resmed shows 5 o rmore AHIs during the same date range.
The Jan 7 AHI's look like they match. It must be an issue with data on the card not being right, prior to Jan 7. The MyAir AHI's do look a bit on the high side. Those numbers are most likely to be correct. It still would be helpful to see your Daily Report detail screenshot for Jan 7. May be able to tell you more from there. Make sure to use the Write a Reply button at the bottom of the thread so you get a full screen width to post into.
Hi Sierra,
Would you please advise about my results? Thanks in advance,
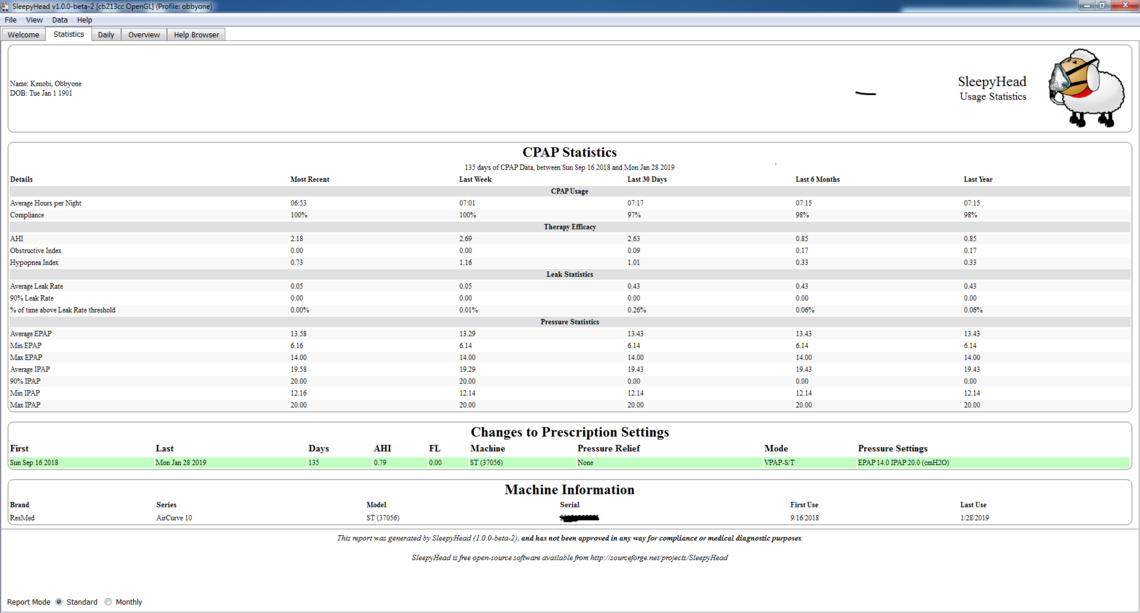
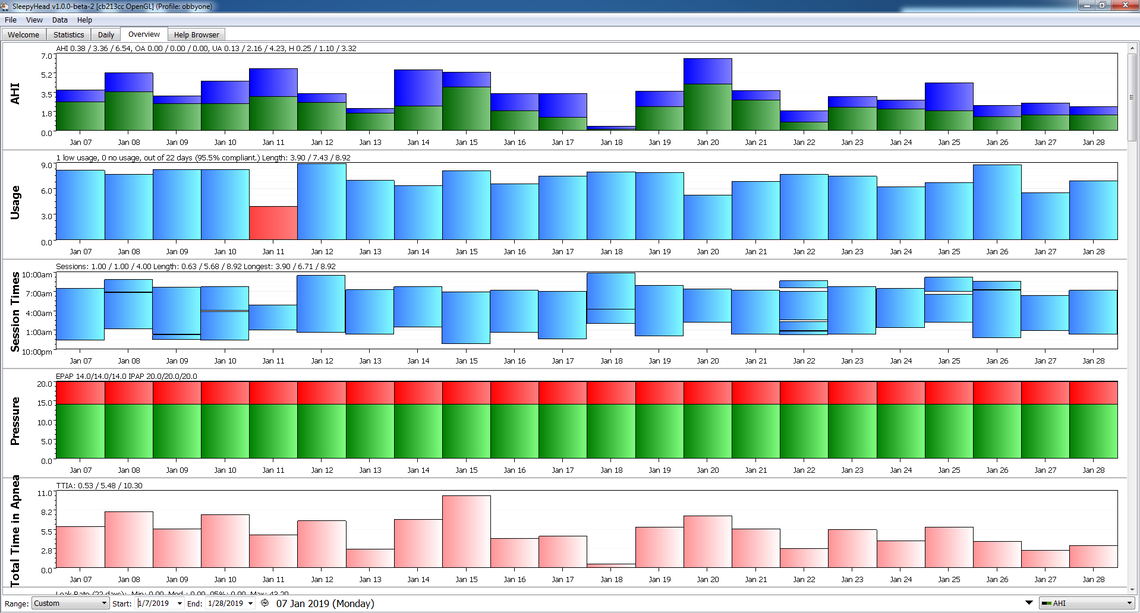
It looks like you now have good data in SleepyHead from Jan 7 on. From what I can see it appears to be only reporting unclassified and hypopnea events. Your AHI is not all that bad. Total time apnea seems on the higher side, but better recently. From the statistics page it looks like the machine is running pretty much at maximum 20 IPAP and 14 EPAP. There is not a lot one can tell from the statistics page beyond that. Similar with the Overview page. To tell more you would need to post your Daily Detail page. Bonjour may be able to help you better than I can with your BiLevel machine. It should be capable of going up to 25 cm of pressure, so the machine is not the limit. Your current setting of max IPAP of 20 is the limit. That said I noticed you reported you were suffering from Aerophagia, and that is often related to pressure. Perhaps once you get used to the pressure, an increase in pressure may be in order.
What if I reach the max pressure? Nothing else to do?
Assuming the machine you have is the ResMed S9 VPAP ST, it has a maximum pressure of 25 cm. You have 5 cm more pressure available to use if it is necessary. See this link to a technical manual. The AHI you are getting is not real bad. Normal target is to get under 5 for AHI. You could discuss increasing pressure with your sleep clinic if they are supporting you.