I have been using cpap since 2004 diagnosed UARS. In Oct 2018 new sleep study diagnosed OSA. AHI 15 RDI 50.8, explains the exhaustion. All drs have commented on narrow airway.
My APAP was set 4-20, AHI 2.8, felt better but not great. Changed the setting 9-16. Since then my 90% pressure went up from 9.0 to 10.5, My sleepiness is not bad most days, AHI 0-1.
Days like today are the problem. AHI 0.43, totally unproductive, tired all day. This happens on the RERA days. The last few hours of sleep I remembered being awake, RERA was 6 events over 2 hours plus 2 hypopneas. I'm frustrated that the apap isn't reacting to the RERAs.
I changed pressure to 10-16, with a 6-10 ramp. I had insomnia every single night at that pressure and couldn't tell if it helped. On SleepyHead it says I have no pressure relief. What is that and would turning that on help with the higher pressures?
Is there a way to get the machine to react faster to events? Both hypopneas the pressure was hanging at 9 and went up after the fact. I've contemplated setting a long ramp 7-14 over 5 hours.
Thanks a lot!
What CPAP machine do you have. Phillips Respironics are known to react slower than ResMed.
In either case speed of reaction can be improved by narrowing the range sol that less increase is needed to resolve events. With a fixed Pressure you need to raise the pressure to prevent the events.
It would be really helpful to know what manufacturer and model of a machine you have. To my knowledge PAP machines may report RERA events, but they do not respond to them with increased pressure. And of course when you increase minimum pressure you are taking manual action which in turn should prevent RERA events from happening. That said I do see RERA flags in my SleepyHead graphs and I am now using a fixed pressure. They can still happen with higher pressures. If you have a DreamStation I believe there may be an option in it to change the sensitivity.
You may be interested in a ResMed article on their For Her algorithm specially developed for what they believe are the different needs of a woman compared to a man. The differences between the For Her algorithm and the standard version are highlighted in the table at the bottom of page 5. Both versions report RERA, but the For Her version is more sensitive to upper airway resistance and flow limitation. It uses single breath data to initiate a change while the standard version uses a 3 breath average and will be slower to react. The For Her version ratchets up pressure in response to apnea in close succession and holds it to a minim for the sleep session. It is more responsive to flow limitation and snoring, and less to apnea. Apnea alone will not increase pressure beyond 12 cm. It raises and lowers pressure at a slower rate. This feature may in fact be an option in the standard machine too, as there is a Response setting which can be set to Soft or Standard. The idea is to prevent arousals. As I understand it the difference between a flow limitation and a RERA is that an arousal is associated with the flow limitation.
The For Her algorithm is included as an option in the specific For Her AirSense 10 AutoSet machine. They sell at the same price, and they can be changed with the Mode setting to the standard algorithm. They can of course be used by men too, if the nature of the apnea they have is more of upper airway resistance and less of the obstructive apnea. The good part is that you can simply try it, and if it works it works. If not you go back to the standard algorithm.
Hope that helps some. Post back with your specific machine and I may be able to add a bit more...
Thanks for your responses! My machine is an older Dream Station. I'm pretty sure it is used, they have removed all data relating to cumulative hours.
Last night 14 FL, 6 RERA, 3 hypopneas, VS2 25 - it is the same thing the not responding correctly. I started snoring as the pressure has increased.
Sierra thank you for the paper. I will read it in depth. My dr spent about 5 min looking at my data and said I was cured and gave me prescriptions to sleep and stimulant to stay awake. I have not taken either. Since my first study, I was diagnosed with hypothyroidism and have a foot injury that prevents me from activity, menopause - gained 12 lbs but much more is body fat.
It sounds from the article that progesterone can help also.
Do I need to see a different type of dr? My current sleep dr is a neurologist. Figure 1 resembles my sleep. Flow rate is very inconsistant with mini apneas all over.
Respironics uses two measure for hours. One is blower hours and it can be reset with the Reset Data command. The other is Machine Hours and it apparently cannot be reset. If you go to the Provider Menu, and then I suspect the Information sub menu, you should be able to view the Machine hours. Not sure if this Technical Manual link covers your machine exactly, but it probably is close. See Page 4-18 for info on the Provider Menu.
I see from that manual that the sensitivity setting that I was thinking of only applies to the BiPAP machines, and it only affects the switch time from IPAP to EPAP.
Figure 1 in that article shows the inhale flow curve flattening at the top. I believe that is how flow limitation associated with UARS is detected. If you have that then there may be benefit in a investigating the ResMed For Her machine. You would probably need to get a doctor to make a specific prescription. If you are due to upgrade to a new machine, it may be a good idea in any case. The For Her machine costs the same as the standard ResMed machine.
I am not a medical professional but if you want to post a typical Daily Report I could give you my thoughts on it. Good idea to post the whole evening, and then a second one zoomed in to show the detail leading up to a RERA event. With a PC you just use the F12 to save a screen shot and then with Windows Explorer drag the saved file to the body of a post here.
I'm lost on how to attach the file.
Do you have a PC? If so, just get the Daily Detail full screen and then press the F12 key. A window will pop up briefly in the bottom right of the screen to tell you where the image file was saved. Open a new post here with the orange Write a reply button near the bottom. Enter a few time to give you some space. Then with Windows Explorer find the file, left click on it and drag it to your open message post here. The file should upload to the post. If you have a Mac, I'm sure the method is similar, but I don't know the specific commands. I think the save the screen command is F8 or Shift F8. And I presume Mac has a file manger similar to Windows Explorer.
SH data is saved as .png, this website won't let me save it here.
I ran as cpap at 90% pressure of 12. Feel a lot more rested. No FL or CA and reduced RERA.
I work 2nd shift and sleep is 2 -10:30. When I awaken I always hear noise in our household. Is it possible it is the noise and not actual RERA awakening me?
Something else must be wrong with posting. I have posted many SH image files which are .png format here. I know that sometimes new members have trouble posting images, and they somehow show up magically many hours later. Not sure what that is about.
Are you trying to copy the .png file and paste it here? If so, that does not seem to work. You have to left click on the file in Windows Explorer and then drag it to the body of an open message.
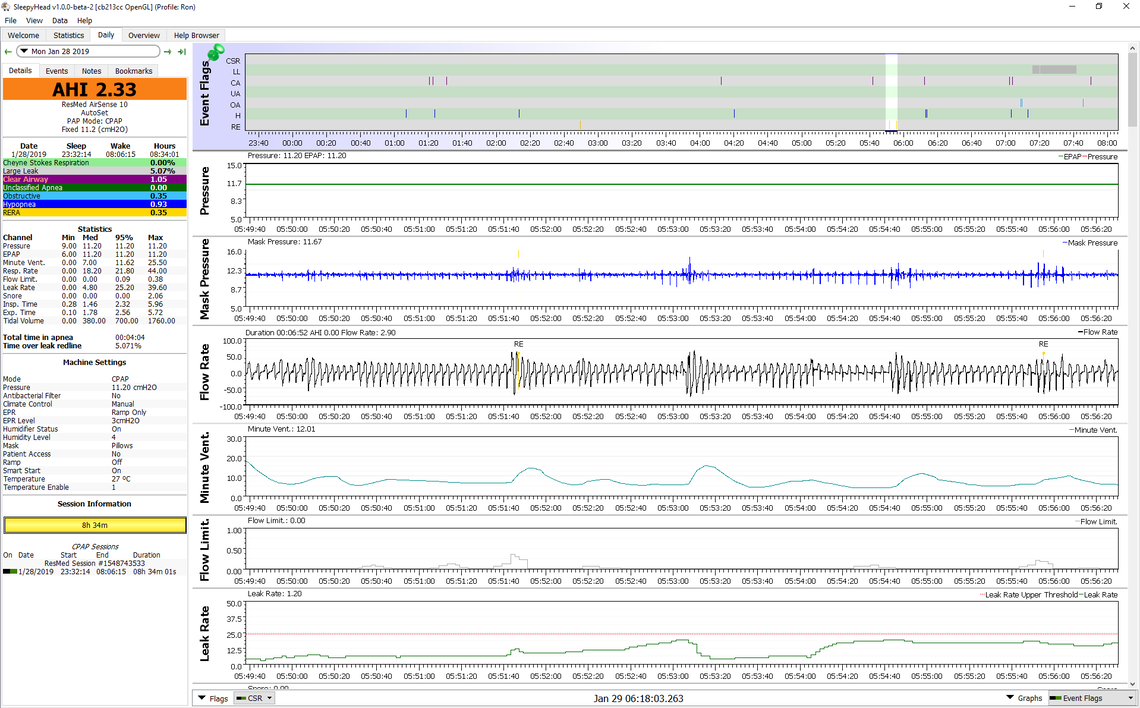
I have switched to fixed CPAP mode as I suffer from mixed central and obstructive apnea, and found an improvement too. It does work for some of us. Noise in the house certainly can be a factor. You should be able to pretty much identify that by the timing in SleepyHead flags for RERA. I don't see any distinct timing of them in my charts. They seem to happen just about anytime. That said I have not done a really thorough analysis of that.
Trying again.
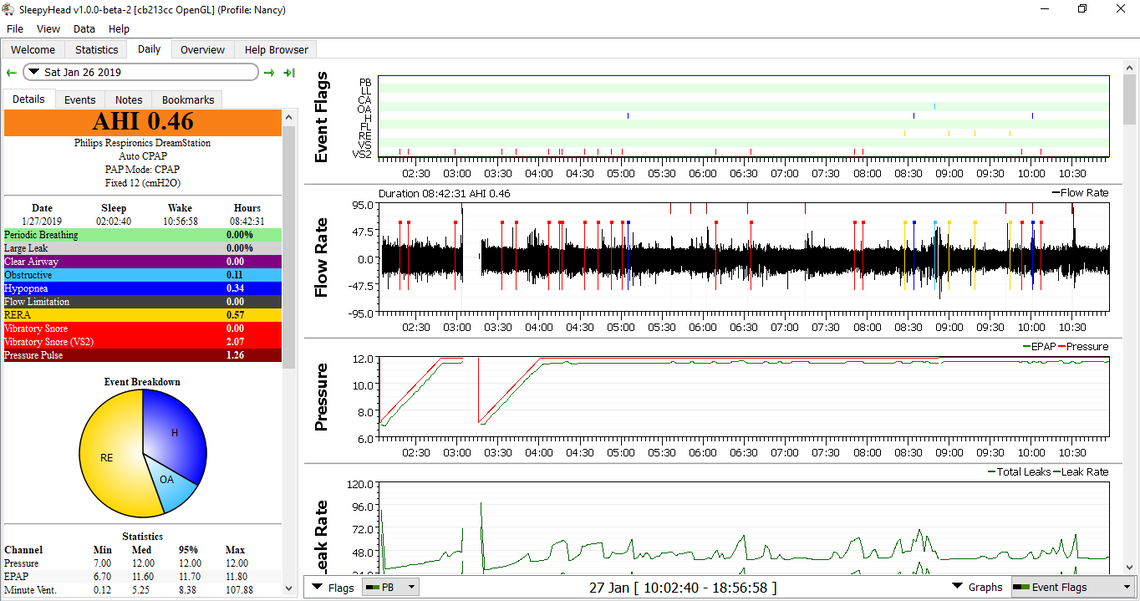
Your overall AHI certainly looks good. The proportion of the RERA does seem high though, and I see it is toward the end of your sleep. Perhaps if you zoomed in (repeated left clicks on the event and or up arrow) on one the events one might be able to tell better what caused it. I like to include what is before the event so you can if there was something else going on. The timing of them may suggest simply noise in the house or lights being turned on?
You could improve your layout a bit to show more data, by going to File, Preferences, Appearance, and then uncheck the box that says something like "show the event breakdown pie chart". It just takes up space and covers up some of the more useful stuff. I also have never seen a good explanation as to the what the VS2 snore means. I think some turn it off with the switches in that box that presently shows PB on your screen, in the bottom left of the graph area. I also like to try to get more graphs on one screen by clicking on the grey dividing bars between the graphs and scrunching them up some to fit more on the screen.
In any case, you certainly do not need more pressure for apnea and hypopnea events. However if you zoom right in on the flow rate data around a RERA event you may see the top or inhale part of the curve flattened out. That can indicate flow restriction, and that may improve with more pressure. I can't quite see the lower leak curve which is the important one with a DreamStation. Sometimes I'm convinced sudden changes in leak rate can wake you up too.
You may be a good candidate to use the ResMed For Her machine. However if your machine is not old and in need of a replacement, that may be hard to justify. It is just going to raise pressure anyway, and if you are OK with the fixed CPAP mode you can do that manually. The advantage of the Auto mode is that it potentially would just raise it for the portion of the night that you need it for the RERA and leave you lower for the rest of the night. Hard to tell without actually trying it.
Thanks so much Sierra. I have 4 roommates who don't have stuff in the morning and the walls are thin. I found today one took off for a month and the other 2 are just not home. They socialize and the house is full of people in the morning. It gives me a chance to see what my sleep is doing without the noise.
I've looked all over the RERA data and see nothing happening. Regarding VS2 I didn't have any until it got cold and I started putting the hose under the covers.
I haven't seen much mention of these in the forum.
Does anyone use them and do they work?
BUG, I think they can be a good idea if you have the standard SlimLine non-heated hose and get condensation (rainout) in the hose. If you have the heated ClimateLine hose they should not be necessary. I use the heated ClimateLine hose but still put it under the covers just to help keep it out of the way.
I think I would spend the AU$79 for a ClimateLine hose before I would spend the AU$42 for a hose cozy though.
It would now be better to not scrunch down the Flow Rate as much. It is OK if AHI slips off the bottom I have not found the AHI graph to be really useful. Also not so much zoom in on that RERA event. It is hard to see the shape of the inhale and exhale flow. If you zoom out and put the RERA event off to the right it should be easier to see if there is any flattening, and if there are any other events leading up to it. Something more like this:
I am 80 and I have been on CPAP for about two years. My AHI's went dramatically down around a median value of 0.50/night. Lately I feel. however kind of sluggish and sleepy until early afternoon, even though I sleep about 8 hours . Looking at my Oscar reports, I noticed RERA episodes, every other day, at around a median value of 0.15. I hardly if ever had RERA episodes in the past. My doctor says not to worry about it. I wonder if it has something to do with the fact that I repeatedly adjusted the min/max pressure settings. They were originally set by my doctor at min 10/max 15. and, looking at the history, there have never been RERA's with those settings. Since last year, I adjusted them to 13-16, 13-17 and lately to 13-18.. The RERA's seem to have increased with the upward adjustments. of the min and max mask pressure values. To day I have adjusted them again to what they were originally ( 10-15). I'll keep an eye on them. May be this was the problem. I wonder if you have any comments.
Thanks
Franco
I very seldom suffer from RERA events. My thoughts are that RERA events occur when the pressure setting is too low, not too high. When the minimum pressure is set low these RERA events can occur before the pressure increases automatically enough to stop them. It would be worthwhile to take note when they occur and what the pressure is at when they happen. With the maximum pressure reduced to 15 cm you also will want to watch how much of the night you are at this maximum pressure and what events are occurring when the pressure is at max. If you post a daily screenshot I can comment on what I see.
Thanks Sierra
Thanks
Franco
Thanks Here is the screenshot . I cannot see any RERA on the event flag graph, only H and OA events. Ref. the min/max pressure settings, I now understand . The AUTOSET feature will work only within these manually set limits.
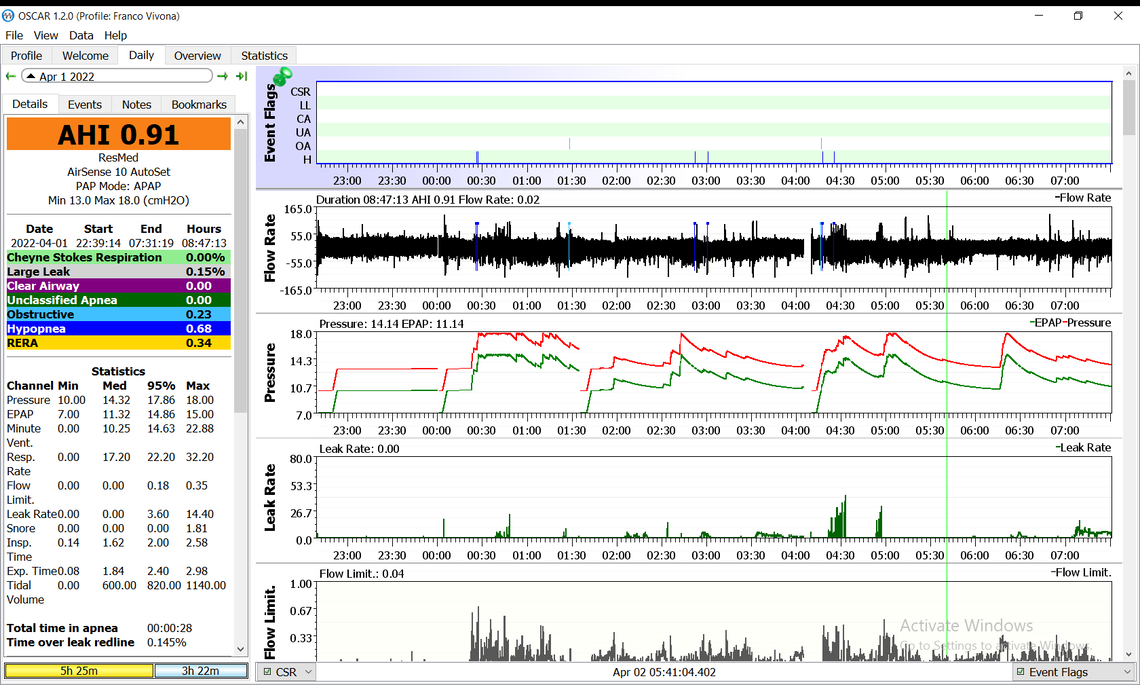
I suspect you may have the flags for RERA events turned off. Left click on the box under the Flow Limit. title at the bottom of the screen, that says CSR. It should display what flags are turned on (green) or turned off (red). Click on the switch to turn the "RE" event flags on. It looks like the first event that started to raise pressure was a hypopnea event. But then the pressure stayed up. Perhaps RERA events were keeping the pressure up. If your minimum pressure was set higher, that initial hypopnea even may have been avoided. It also looks like you are having significant flow limitations. That also may be driving the pressure up.
Thanks
By clicking the CSR box the RE flag line pops up in the AHI events graph, but no RE marker appears. Looks like there have been none, contrary to what the summary shows.
The 10( min)-15(max) value to which I reverted today was the one originally prescribed by my doctor. and there never were RERA's associated with this setting. This is why I thought I would go back to it, but if you have an alternate suggestion, I am open to it, bearing in mind that the settings historically showing a possible correlation with RERA events were those comprised within the ranges 13(min) -18( max) or even 18.6 ( max) .
Franco