I'm looking at getting the ResMed Air Sense 10 in the near future. It looks like my doctor is willing to write the prescription based on my 18.1 RDI and 4.7 AHI. Pretty sure that it is Upper Airway Resistance Syndrome that has been causing me fatigue and poor sleep all the way back to early teenage years. Sleep efficiency was listed at about 40%. for the first sleep study that only resulted in under 3 hours of sleep. I feel like a truck ran over me in the morning, basically. Don't want to get out of bed, exhausted whether I sleep 6 hours, 8 hours, 10 hours or 12 hours. I feel a little better with more sleep, but still exhausted all throughout the day. I fall asleep in my computer chair a lot, sometimes as a passenger in a car, don't have enough cognition to be confident that I'm not going to crash into someone while driving, etc. I'm still going to see about having another sleep study because I want to make sure this isn't something like Central Sleep Apnea. SPO2 drops aren't going that low (typically low to mid-90's).
I'm investigating odd "jumps" that don't occur that frequently throughout the day. If something brushes/touches my hair, for instance...my whole upper body reacts with a "jump" that comes from what I believe to be my back area. Neurologist said I'm fine and everything seems normal. She said to get an MRI of the back for that, which I will do at some point, but I seem more twitchy like that when I'm really tired. It makes it worse for some reason.
I'm curious how the autoramp settings work. Does it start out on a very low setting adjust itself up until it feels no resistance and stops at that setting?
I'm reading conflicting reports all over the place about what it can and can't monitor. What things can it monitor?
The Air Sense 10...some people say it is hard to clean the tank. I have seen lots of commercials with what I felt was scam-like products for "cleaning" the mask, tubes, etc. Some kind of device that you just attach the mask/hose to and run something through it for a while to "clean" it. Realistically, what are the chances of getting sick over different time intervals?
Based on all your symptoms, I hope you can get the For Her version of the AirSense 10. That mode could work well for you.
When you set the Ramp to Auto it essentially holds the pressure at the Start Pressure until it detects you have gone to sleep. When you go to sleep it then ramps up to the Minimum Pressure. One of your issue may be that you do not need a lot of pressure. You cannot set the Start Pressure any higher than the minimum pressure. I would discuss the setup with the clinic and try to get them to put the minimum at no less than 6 cm at least as a first try. If they put the minimum at 4 cm that can feel a little suffocating. When you use the Auto Ramp it also makes sense to turn the EPR on, set the type to Ramp Only, and set EPR to 3. That way it will cut the pressure back on exhale while you are awake. That makes breathing easier. For example with a start pressure of 6 cm it will cut back to the machine minimum of 4 cm on exhale, and still give you 6 cm on inhale. Hope that makes sense.
Cleaning is no big deal. I use pure household vinegar to clean the mask, hose, and humidifier tank. Then I follow that with Dawn dish detergent and water to get rid of all the vinegar. Last is a clear water rinse and then hang to dry, except for the humidifier, which you just need to refill with demineralized or distilled water.
What's cm as a rating? Centimeters? Cubic meters?
Is that cleaning once a week and just a wipe down or do you soak the hose/mask and fill the tank to sit for a little while before wiping it down?
The odds of getting the clinic to help me with settings are probably going to be low given that they don't want to help unless I buy one from them for like $1,800. I see the Air Sense 10 online for as low as $600, but of course I would still need to get the mask and such.
The full units of pressure are cm of water. Many get lazy and just say cm. Google tells me that a professional trumpet player can blow about 130 cm of water pressure. An APAP like AirSense 10 produces a minimum of 4 cm of pressure to a maximum of 20. It is a very low pressure. Don't hire a trumpet player to fill in if your APAP breaks down...
It is recommended to clean your mask daily by just wiping with soap and water. ResMed sells special wipes, but I think they are unnecessary. I have a full container of them that came with my package and I have never used them. The hose, and humidifier is generally recommended to clean weekly, but I suspect many of us stretch that a bit.
The For Her version should be the same price as the standard AutoSet on line. I would look for a package that includes a heated ClimateLine hose. It is not essential, but nice to have. If you are going to set up your own machine I would highly recommend using SleepyHead to monitor your results. The initial settings are not that difficult. Out of the box it will be set to a minimum of 4 cm and max of 20 cm. Not a good idea to leave it with those settings. Based on your low AHI I would suggest a minimum of 6 cm and max of 10 cm, along with the comfort settings I gave you above. With a week or so of using it, you most likely could reduce that maximum pressure limit. Keep in mind that the machine will only go there if it sees apnea events. SleepyHead will tell you exactly where the machine takes the pressure through the night.
I guess the other thing that I've been pondering is...how do people get "used to" the fact that they are relying on a machine to get proper sleep every night? I'm not married, but plan to be at some point. I'm sure that's a big factor for many people. Probably takes a while to get used to having something crammed into the nose (nasal pillows) or pressed tightly against the face (mask), I would imagine. Then you have to keep up with how old the machine is, if the power will stay on during storms (though I understand that some have a backup battery), etc. How do people keep alert enough to drive during the time when they're getting used to the CPAP, for instance? My AHI is considered "mild"...but I'm definitely not alert enough to drive. I work on large machinery at a manufacturing plant and I find myself having trouble staying focused in general to watch the machines that I'm supposed to be watching. I just get distracted by the wrong things and it is because my sleep is so horrible. From what I've read, it takes a while to get used to this.
A few comments. First a PAP machine is not really a critical life support system. It can fail and you will still breathe, perhaps a little uncomfortably, but you will still breath. My wife's machine had a problem with the power supply cord and it went off on her several times one night. She was a little ticked off, but nothing more beyond that. A back up power supply is not necessary, unless you are living in an area where power goes out daily or nearly daily.
It will take some time, but I suspect you will get used to the machine. In my opinion the nasal pillow mask is the least intrusive. I recommend it as a first try, and even if it requires mouth taping, it is better than a full face mask.
Your machine keeps track of operating hours and you can check it anytime. In general they last 5 years or more.
I would expect once you settle into the treatment that you will be getting a better sleep. I think part of the trick is to focus on getting 7-8 hours of uninterrupted sleep each night with no naps during the day. It may not happen from day one, but it is good goal.
Somewhat of a guess at this point, but I suspect you will only be needing a fairly low pressure and it should be quite comfortable and fairly easy to get your mask to seal. On trick however is to not set it up too low. That can give a suffocating feeling while falling asleep on in the night when the machine backs off the pressure.
Best to go into it with a positive attitude and come back here for help and support if issues arise. Everyone's experience is a bit different. My wife loved her machine right away. It took me a while to warm up to it.
Hi again Singingkeys
Sierra's encouragement to remain positive is worth noting.
It might even work for you but am I allowed to have a doubt or two?
Yes the CPAP should solve mild apnea fairly easily and even if it doesn't it's only mild.
My concern would be that your symptoms seem to be excessive for mild apnea.
You may have to solve more than just apnea before you get the outcome you want.
My concern would be that your symptoms seem to be excessive for mild apnea. You may have to solve more than just apnea before you get the outcome you want.
Well, I've been to an ENT doc, have had an MRI of the brain (normal) that happened to pick up a deviated septum with side spurring. So the ENT doc saw that and requested a CT scan of the sinuses. Swollen turbinates and deviated septum. Corrected via surgery and successful in July 2018. That made the airways in my nose too small, so it basically took long to inhale/exhale and made that easier. However, it didn't improve my sleep. Didn't want to bother with UVVV surgery - far too risky and I've known two people (one of which nearly bled to death) that had it done and it failed, so they had to go back for emergency procedures to stop bleeding. Didn't want to mess with the mouth device...looks very uncomfortable/possibly worsens TMJ (which I already have a bit of) and moves teeth. Had a lot of dental work in the past and don't want to move anything around again. Then there was the neurologist. We didn't get to the MRI of the spine because my insurance had a ridiculous amount of stuff going through it and they didn't want to pay for anything else. I went to the primary care doctor before all of the above and they checked a full blood count, thyroid check and all of that. It was all normal. My heart rate tends to be up during the day when I don't sleep well and I will also have some nights when I'm going to bed and I feel like a pressure in my hands and/or face like my blood pressure is high during those specific two areas only. But when I check my blood pressure with the auto machine that I have, it is normal.
My concern is the "jumps" and there have been times in my sleep when I have had those (possibly just hypnogogic), but not that much. I also get them during the day on certain days and they are core jumps. I'm much more jittery/jumpy when I'm tired in general. I'm still in the process of researching another sleep facility in my area that will check for some of the other things that all of them don't check for and will consider RDI in diagnosis. I have a light essential tremor/shakes that I have had since I was a kid. I have always been very "jumpy" in general in regards to random jerks. A solution was never found. So I'm puzzled. With such a low sleep efficiency and a moderate RDI, I feel so bad for it. Running out of options.
Wow it sounds like you've been through the works!
Whatever happened to boring stuff like EBV, PTSD, CFS or whatever other acronyms are out there for the Vague UnDiagnosed Stealth Disorders. VUDSD (my creation) :)
My high RDI and low AHI still seem to point towards UARS, as Sierra has suggested before. I have found direct evidence in research online where articles specifically state that UARS is usually the case when there is a high RDI and a low AHI.
Without a doubt, something is seriously wrong with me. Around the beginning of 2018, I was having feelings in my chest kind of like a cramp, but I also felt like I just couldn't get enough air and constantly yawned, got chills and such. When they did the blood draw at a clinic, I fainted for 15 minutes and woke up with blood everywhere and the whole clinic staff in there. Blood pressure shot down to 60/60 and 52bpm pulse. I've never faint or had any issues with blood draws and I have had a ton of them throughout my life. I even followed up at my primary care doctor a day or two afterwards and had a blood draw with no issue whatsoever. A lot of people have told me that tiredness from sleep apnea can't cause fainting. No cause for that was ever known and doctors basically swept that under the rug as one of the "we don't know what happened" things. Haven't had issues since, but I do feel heart flutters/palpitations on days when I don't sleep that well. I might "get" 7 hours, but at 40% efficiency, I'd be getting more like 4. So yeah, I hoping to get to the bottom of this. I could get the prescription right now based on the previous sleep study, but it sounds like I might have a little more going on. That kind of scares me to just get a machine and assume it will take care of everything. When I'm really tired and just sit back in my chair upright and doze, sometimes I feel like drifting off to sleep upright closes my airway until I pop awake. But other times, it literally feels like my lungs just don't want to use up the energy to breathe hard enough, so I'm wondering if my breathing doesn't get shallow for some reason while sleeping. That may just be because I have compounded so much tiredness over the years that I'm running on empty for energy, but who knows. Meanwhile, the study can take a peek at the EKG and all of that at the same time.
You've come a long way already Singingkeys
Keep at it and you have to get answers eventually.
In your circumstances I would prepare a document with my medical history laid out as concisely as possible so that everybody I see will be able to embrace the whole picture and better understand where to look for the missing pieces of the puzzle.
It also helps me when at critical appointments because I am often too tired or confused to remember details or even make much sense especially if it goes for too long.
i was told i had severe sleep apnea three years ago, here i am three years down the road using cpap still tweaking here and there,cpap does not just help mild sleep apnea. i had 56 events an hournow my ahi is o.1 so dont be negative about cpap i dont know about anyone else it works for me, i have good nights and bad nights so i will leave you with the words of spock live long and prosper.
The hardest part is that I just don't know what I have that is making my sleep bad. That last study...I honestly didn't even remember going to sleep at all that night, but they said 2.75 hours. It seemed like I laid there the whole night awake. Their graphs showed different stages of sleep. I think the 40% efficiency is probably right. That's about what it feels like.
I can get the CPAP prescription, but what if I have something like Central Sleep Apnea? It can be hard to concentrate on work sometimes because I'm so tired and not alert, but yet that's the work that will give me the money for a sleep study to start treating it, so catch-22. If it is Central Sleep Apnea, I see where CPAP is used to treat it sometimes and them BiPap at other times. Tax refund time is coming up, but that's weeks away at least and the government shutdown is making it take longer. :-/ But if I get CPAP and it doesn't work, I'm back to square one and still not sure what the problem is.
If we consider possible UARS or CSA...is there anything else besides OSA that would cause all of this?
It seems to me that either I am not thinking straight (which is very likely) or you have perhaps tangled too many things together.
There is being tired all the time
There is not being able to sleep
There is apnea
They are not one and the same.
Perhaps you need to follow some advice that Sierra gave to me a few days back. Look at them one at a time.
Yes there are connections and one can lead to the other but apnea does not really keep you from sleeping. (sorry I meant getting to sleep) (added later)
A few days ago you reported that you had a RDI of 18 and AHI of 4.7. Do you know what the breakdown of events that made up the AHI? If there were no central apnea events in the diagnosis, then it would seem unlikely you are suffering from central apnea.
An APAP is most likely to bring the RDI and AHI down, but you don't have a lot to come down on the AHI. Most of your potential improvement would come from reducing RDI. The APAP is most likely to do that too. The real issue is that there certainly will be some disruption of your sleep at least initially when using an APAP and mask. Will the RDI reduction be enough to offset the effects of having to wear the mask? Hard to predict. You most likely will not need a lot of pressure and mask leaks should not be a big issue. It is unfortunate there is not some way to do a trial to see if it works. The proof is always in the pudding.
Well, my respiratory data was quite interesting:
As we noted, 13 unclassified hypopneas added to 37 RERAs in the 2.75 hours of sleep. They base their hypopneas on 3% or greater desaturation. I also see 41 snoring episodes 14.86/hr snoring index. I didn't hear that much snoring when I have recorded myself, however. In another area further down, they noted 45 RERA's.
Interesting, for "Obstructive Hypopnea" and "Central Hypopnea" they had 0 for both. Mine were unclassified at 13. If it isn't central or obstructive, what the heck else is there? I would guess something like neurological, but they also noted that there were no PLMS (Period Limb Movements of Sleep).
I'm definitely not as alert as I should be and I am nothing but purely tired from the moment I wake up until the time I go to bed. Curiously, my lips always feel super chapped and are visibly red for a lot of the day even when they aren't physically chapped, as if my blood pressure is up or something. Yet it tests fine when I check it and my blood pressure is normal with a pulse rate a little higher than normal. I'm to the point where I'm about to just ask the sleep doc for the CPAP prescription and buy my own online. I saw one sight where they had it for about $600 and of course I'd need the mask and whatever other accessories, so probably $700-$800 and just start trying it to see how I do. My sleep is not restorative at all and I just fall asleep in my chair every single day watching a 10 minute video on the computer. Until I can pay for an actual sleep study later to find out exactly what is going on, I may have to buy one to get me through. I'm having major concentration problems now and even on days when I can sleep in, it is like my sleep isn't working to recharge my body. I wake up with red lips, puffy/red eyes that look swollen and I have no energy. Just isn't happening.
"Interesting, for "Obstructive Hypopnea" and "Central Hypopnea" they had 0 for both. Mine were unclassified at 13. If it isn't central or obstructive, what the heck else is there? I would guess something like neurological, but they also noted that there were no PLMS (Period Limb Movements of Sleep)."
I recall that got discussed in one of your earlier posts. It is my view that there are both obstructive and central hypopneas, but it is difficult to distinguish between them without a lot of manual effort. For that reason I suspect few sleep labs actually do it. One can sort of do it with a lot of effort using SleepyHead, but it would be a pretty time consuming exercise. My thoughts are that one quick and dirty way to estimate the obstructive vs central hypopneas would be to proportion them in the same ratio as obstructive and central apneas. In your case all apneas are obstructive, and there are no central apneas. Using my seat of the pants guestimate method, that would indicate all of the hypopneas are obstructive in nature. In effect they are a flow limitation that does not proceed to full obstructive apnea.
As an aside with a CPAP, apneas can be designated as unclassified. That is a bit different. At least in the ResMed machines they mainly use that unclassified category when there are mask leaks so high that accurate classification is not possible.
You have a difficult choice to make, and I would not want to push you in one direction or another. If it was me, and it was going to cost me as much for another sleep study as it would to buy a machine, I think I would lean toward buying the machine. If it turns out to be a bad solution, then there is at least the possibility of selling it to a place like SecondWindCPAP.com, and getting some money back.
I can't remember if I posted the technical paper on the For Her version of the AirSense 10 AutoSet. Here is a link to it again. The reason I think it may work for you is that it puts more emphasis on flow limitation, and snoring, and less on full apnea. That seems to be your situation.
A little further research revealed that hypopnoeas are only classified as either obstructive or central in paediatric studies. In adults they are just hypopnoeas. We don't do paeds here so I had not heard of that.When it comes down to it, the classification of an event is far less important than whether CPAP makes it go away.
I'll try to get the For Her version and start out with a nasal pillow mask as soon as I can buy them. I'm going to try to get the prescription from the sleep doctor tomorrow so that at least I'll have that. One of the things concerning to me is that even sitting up in my chair or laying down in the bed during the day for a quick snooze...I reach a point where I feel like my lungs become "lazy" and just don't want to breathe very hard or they just prefer the "relaxed" feeling of resting/not breathing vs breathing. It just feels like a lot of work to breathe for some reason, so my breathing becomes quite shallow and I'm not sure if it is keeping up enough to provide my body with the right amount of oxygen needed while I'm sleeping. I've never had any lung issues, so maybe that is just like that because I'm so tired and that's how my body responds. I hope I'm not doing that all night, though...like shallow breathing that gets smaller and smaller in breaths until I just stop breathing because of that feeling of the lungs. If I went to a pulmonary specialist, I would probably pass every test and they would say that nothing was wrong with me, so that's also discouraging. Maybe it is just a byproduct of not sleeping well enough and so when I do start resting it feels like I'm not getting enough air in general. I yawn an awful lot throughout the day. If I'm active, then I remain active...but if I sit down, I want to fall asleep. At the follow-up appointment after the sleep study when the sleep doctor told me that I didn't officially have sleep apnea...he also noted that it "was a good thing that I had a job where I was active and moving around, because if I had a desk job, I would be falling asleep." Boy was he right about that. I presume he was going off from the 18 RDI alone and the unclassified RERA's. That was when I had a job where I was walking 5-8 miles a day. At work, I have a fast-paced manufacturing/production job, so I am physically awake...but I wear down quickly and I'm not as alert. Sometimes I feel like there's a little fluid in my lungs or something (almost like I feel a slight rattle when I breathe sometimes), but only on days when I don't sleep very well. I'm not one to get sick with a lot of colds/allergies or anything.
I found an Airsense 10 Autoset For Her w/ HumidAir for $659 new. They have some other accessories and add-ons to pick from. That's the lowest price that I have found for a new one (absolutely not buying used) online. That's a whole lot better than the $1,800 or so that my sleep doctor wants to buy it from their facility. Even the lady working there told me to buy it online because their price was ridiculous.
The one good thing about getting a good machine like the ResMed For Her is that you essentially get a basic sleep study done every night you use it. The machine will easily detect central and obstructive apneas, RERAs, and Hypopneas, as well as snoring and flow limitation. It is all there to see with SleepyHead. It is a significant price to pay, but it may be cheaper than another study.
That's probably best, anyway. I can be at home in my own bed and don't have to ask a sleep rep to get up and go to the bathroom or whatever. They literally had an attitude whenever I asked for someone to come unhook me when I needed to go to the bathroom. Then I read later that constant arousals like that actually cause you to have to go more often, which they obviously didn't know about or they knew and didn't care. Sounds like I just had a horrible place to have a study at, but that was the place that was recommended. Alright, that's going to be my goal, then.
So it looks like I'm going to need:
The machine itself, a hose, a mask, filters and what looks to be distilled water for the humidifier built in. Am I missing anything else? Going to start prepping a list. I see that on the website I linked to above, it says I need a prescription to buy a mask from them. Sounds a bit ridiculous. I'm going to have to figure out a way to have the sleep doctor write a prescription for the machine and a nasal pillow mask to start with (or is the machine prescription itself a catch-all for all accessories?) and then if I think I need a different type of mask later I might have to ask him to write one for that.
Yes, you need the machine, and the basic package should include SlimLine tubing, the power supply, the humidifier which is built in, the SD Card, one filter, and a travel case. Some places will put together a few more things in a package, such as extra filters, the heated ClimateLine hose, and sometimes a choice of a mask from a limited selection. These can be a good deal when you add it up. Even if you have to buy it as an option I would recommend the ClimateLine hose. It does add to the comfort factor, and makes it easier to get the humidifier setting right. Some like to add in the SoClean machine and I think that is a bit of a scam and not worth it. Distilled water you can get from places like Walmart etc.
On the prescription I doubt that anyone would prescribe any specific mask, and you wouldn't want them to. I would think just a prescription to use a CPAP is all you need. Perhaps call a vendor you are considering using to ask what they want for a prescription. I suspect what that site means by saying they need a prescription to buy a mask, is that they are making the point that you need a prescription for a CPAP to get a replacement mask. It seems to be a goofy US rule. It is not a requirement in Canada. You should not have to get a prescription for each mask you buy. Perhaps if you can get as bonjour suggests just a prescription for the APAP and mask of choice you will be good to go.
On the mask, if you just have to pick one without trying it ahead of time, I would pick the ResMed Swift FX nasal pillow, or the ResMed AirFit P10 nasal pillow. They are two of the lower priced masks and typically get good reviews for comfort. The head straps on the P10 are somewhat flimsy and are not that durable, and can have issues with keeping the mask in place. The P10 has a very quiet exhaust port though. The headgear on the Swift FX is more substantial and I suspect will last longer without replacement. The Swift FX exhaust port is not as good as the P10 but it can be worked around. I've used the P10 for about 9 months now, and have just replaced it with the Swift FX. For either one if you are just buying them on line make sure you get the fit pack version. It includes three sizes of nasal pillow inserts.
They both come in standard and For Her versions. I would buy the standard if you are male, and the For Her if you are female. In both versions the nasal pillow inserts for the standard version are small, medium, and Large. In the For Her version they are extra small, small, and medium. The headgear on the Swift FX For Her is a bit smaller than on the standard. On the P10 I believe the headgear size is the same on them both. It is very elastic, and part of the reason why it is kind of flimsy.
Hope that helps some,
So when I do get a machine and start getting proper readings to find out exactly what I'm dealing with and why my sleep is so non-restorative:
Whether it is Obstructive Sleep Apnea (which I understand to be the airway closing off with or without oxygen desaturation), Hypopneas (abnormally slow or shallow breathing), RERAs (simply being aroused lots of times due to being awakened to breathe), UARS (narrowing/collapse of the airway to cause RERA's/Hypopneas), or snoring...is APAP pretty much going to be a "stuck for life" thing? How do people get over the shock of that? A lot of people say APAP/CPAP is like a bandaid cover for the problem instead of fixing it, but in actuality, I'm not seeing those same people stating an actual solution that works. Is it just non-existent in today's medical world?
I'm a little familiar with UPPP, or (Uvulopalatopharyngoplasty) aka Sleep Apnea Surgery where they remove tonsils, scrape extra tissue from the back of the throat and remove the adenoids. Doesn't seem to stop people from having sleep apnea and is very dangerous to have or can cause even worse problems with breathing, eating and speaking. I have read where some people go as far as to have their tongue basically cut and moved forward in their mouths because they felt like the tongue fell back and blocked the airway. I've had my turbinates reduced and also deviated septum fixed and airways enlarged. Didn't help my sleep issues, but helped my general breathing. For something like UARS, I'm not aware of anything they can do to physically help an entire upper airway that could be collapsing/narrowing, for instance. I guess they could attempt to put some kind of permanent tube in it to keep the airway open (much like tubes in the ears)...but doesn't sound feasible. If it is RERA's that can't fit into the Apnea or Hypopnea categories, is this going to end up with neurology and taking a pill for life instead of APAP? Will there be no physical way for me to stop using the machine when an issue is discovered for sure?
Just trying to get my mind used to what it will be like tethered to a machine for life. It gives me sort of the mindset of being naked and vulnerable in life because I'd be depending on a machine to sleep properly. Granted, I will of course need to try it anyway. My girlfriend has a disability (sleep terrors and possibly another sleep issue), but we don't live together. Her dad has OSA for sure. She says she doesn't have it, but I wonder if she actually does in some form because I have read that night terrors can have links to it. Apparently she wakes up screaming and such, struggles with anxiety and a variety of issues. Then I picture if we ended up getting married someday...both of us would have sleep issues and literally have to have separate beds to keep from driving each other crazy with our sleep issues. Yikes. That's a lot to process.
Methinks you think too much singingkeys!
And ask way too many questions that are far too hard to answer! :P
And I only have a couple of dysfunctional neurons left and they have quit for the day.
Yes it is a lot to deal with.
Too much!
I hate feeling compelled to quote Sierra but he branched out into elephants and boxes at some stage and it really made sense and in this case it might be the safest way forward.
I tend to overthink. It's just one of those things for me, I guess. For instance, I already require glasses/contacts just to see properly. Both of those are "tricky" because you have to get a new prescription when the old one expires and the new optometrist may not be as lenient as the last. One eye is different from the other and they always want to make them different when I go to a new person, but it causes headaches. So they play with the prescription and I end up going back getting them both corrected to be the same for both eyes. I guess I feel like this could be the same way for APAP and sleep stuff in general. You get the right prescription you need and then it expires in x years and you end up having to have another study or the same doctor isn't there/retired or whatever. Then you jump through hoops to get what you need again. Probably will need to start wearing a mouth guard soon. I also have trouble with my legs and walking is even more uncomfortable on the days when I don't sleep well enough. Everything seems like it is "tricky" and a handicap of some sort to always make life a little more difficult, as if it isn't already. lol
I guess I feel like I'm falling apart sometimes or something. :-/
Example Link TextExample Link TextLife is perilous for sure but I wonder if it's the peril and stress that make it actually living.
I suspect the best way to face life and make it work for you is to embrace the stress and uncertainty and difficulties as challenges like a game.
You are obviously capable of doing this as long as you keep moving forwards and don't let it overwhelm you.
Yes it sounds a bit pompous sorry.
Especially from someone who is convinced that Murphy has a personal vendetta against me and routinely tries to anticipate Murphy's next move and change my plans to circumvent it. :O
Ah, good 'ol Murphy. Fortunately I haven't had him visit me too much. I guess we all just have our own burdens to deal with.
Lol it's the same as fate or karma or any number of names for an instinctive calculator of statistical probabilities many of which become self fulfilling prophecies.
I have lived my life as an opportunist and risk taker and generally made it work for me especially when I was younger but it seems that for me the odds are at their worst when there is a potential for impacting on others or when the plans depend on others.
I guess it's the balance for the risk taking file.
An instinct that if the risks are too great and the potential disaster too extreme being overconfident (or depending on others) would be just begging for something to go wrong.
Double the risk = double the precautions.
Hi, my name is Jeanette. I have just been diagnosed a few weeks ago. So I sleep with my cpap machine and my husband sleeps with his.. I have severe sleep apnea but with losing weight I am lessening off the pressure by just a little bit.. I feel like I am buzzing and it wakes me through the night.. so nurse said to try turning it down a little.. We would look a funny / scary sight if anyone came into our room...
Hi Jeanette.
I was so looking forward to creating chaos in that topic that you didn't start. :O
On the subject of partners my wife is starting to sound like a cross cut saw, which I find rather cute, but I wonder if I will ever be game to broach the subject with her of doing a sleep study.
We see people getting married and then trying to marry off their friends and then they have babies and encourage their friends to do likewise which, for a cynic like me, seems a bit suspect and I worry that I might be doing the same thing, by dragging my wife into the world of CPAP.
There are times when it's not nice to share. :(
Hi Jeanette,
I think I saw a post you made in the Introduce yourself thread. Have you heard of SleepyHead software? It enables you to see the detailed data on your machine. It is not the greatest idea to just reduce the pressure of your machine without having any way to monitor what it is doing. If you need help using SleepyHead perhaps just post in the new thread...
About the only way to reduce the effects of apnea and possibly get off the PAP solution is weight loss if that is an issue. Males with a neck size greater than 17" and females with a neck size greater than 16" are at high risk for apnea. In many cases significant weight loss would bring that down. But, then there are others that are not overweight and still have apnea issues. Those tend to be more likely to suffer from central apnea, which is a different kettle of fish...
I am a guy, 5'8 and 160 pounds. My neck size is 15.25". I could lose 10-15 pounds and still be within a reasonable weight amount, but I'm more stocky/muscular and probably 10-12% body fat. I used to lift weights a lot and such back when I actually had the energy to do so. That sounds more like what I fit in with...not really overweight and still have issues.
A few posts back you asked this question:
"If it is RERA's that can't fit into the Apnea or Hypopnea categories, is this going to end up with neurology and taking a pill for life instead of APAP?"
Not a medical professional but I do get RERA indications on my ResMed AirSense 10 machine. This is how ResMed defines them:
"Respiratory Effort Related Arousals (RERAs) are periods of increased respiratory effort leading to an arousal. Increasing respiratory effort will be seen as airflow limitation. These flow-based RERA events are logged and stored as summary and detailed data..."
I am not totally sure how the machine can tell that an arousal occurs. When I look at the detailed data in SleepyHead when a RERA is flagged sometimes I see something that looks like an arousal (disruption in flow rate), and sometimes I do not. What I do see fairly consistently are indications of Flow Limitation.
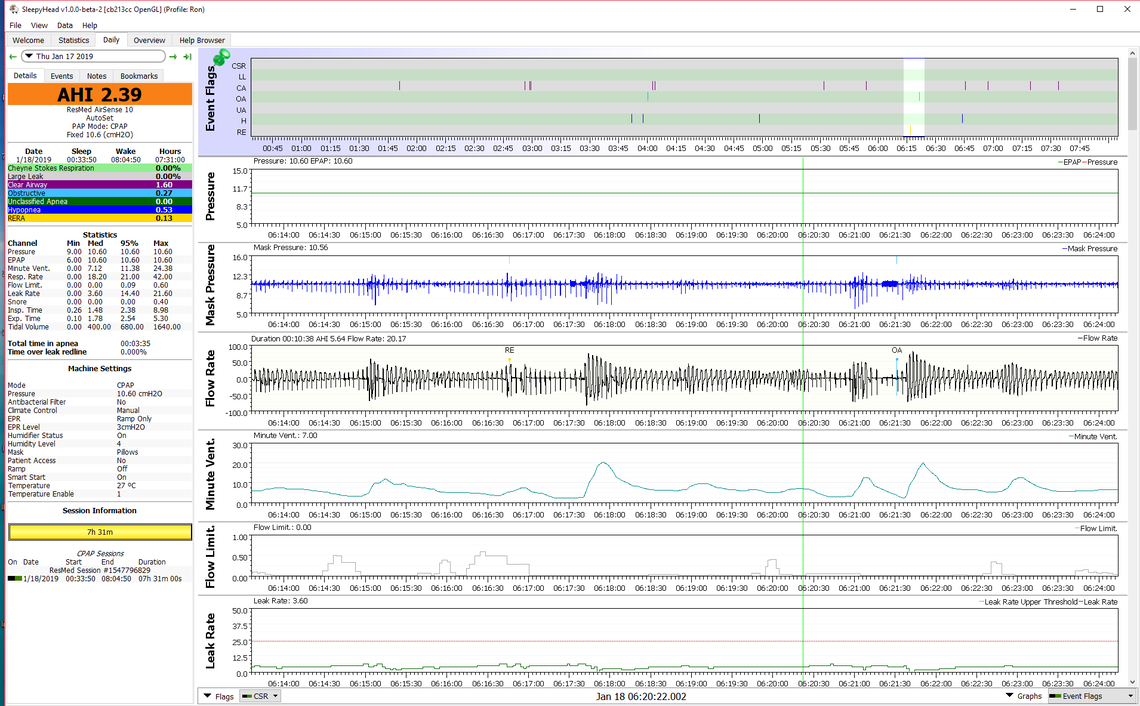
In any case here is an example I found in my SleepyHead file of an event which includes both a RERA and an obstructive apnea. The RERA event (flagged as a RE) is associated with a quite significant (for me) Flow Limitation indication. This is followed by a fairly significant drop in Minute Ventilation which is amount of air being breathed in and out. Blood O2 levels tend to follow Minute Ventilation. The RERA event is fairly quickly followed by a non flagged obstructive event at 06:17:30. I can tell that by the blob of blue on the Mask Pressure. That is showing the machine is cycling the pressure up and down to sense whether the event is obstructive or central. It does not reach the 10 second of duration so is not flagged, but it occurred. When it ended there was a big spike up in Minute Ventilation showing over breathing to compensate for the period of reduced air flow.
Things kind of settle out for a while after that, but at about 6:21:30 an obstructive apnea is detected and flagged this time. The blue blob is longer and the event met the minimum of 10 seconds criteria to flag it as an OA. You can see it had essentially the same impact on Minute Ventilation reduction as the RERA did, so probably the same impact on oxygen desaturation. If anything the Minute Ventilation was reduced for long as a result of the RERA than it did for the OA event.
Sorry for the long drawn out explanation, but the point is that RERA is not a lot different than a full obstructive apnea when you consider the impact it may have on Minute Ventilation, and as a result blood oxygen, and sleep quality. Also, from what I can see in my personal results a RERA is not really associated with a central (open airway) issue and is more obstructive in nature. For that reason a PAP device is likely to treat it sucessfully with pressure. My machine is set to a fixed pressure and did not respond. In Auto mode it would have responded to the Flow Limitation and bumped pressure up. And, the For Her algorithm would have bumped it up even more. That in turn could have prevented the OA event that followed. Hope that makes some sense. Any questions, just ask...
I guess at this point it doesn't so much matter what exactly is happening as long as I can identify and the machine helps. What I think happens is when I lay down and go into a deeper sleep stage, my soft pallet relaxes and becomes sort of flappy-like. As best as I can tell, I feel a little better when I sleep more on my stomach and turn my head to the side compared to just on my back. There have been a lot of times when I woke up and my brain was awake and alert enough to think it was my upper throat closing over and yet my body was still asleep and relaxed to the point where I could simply lay there and recreate it within seconds by letting my throat relax. At that point, it feels like the soft palate closes over my airway in what seems like a flap-like fashion. I'm not sure, maybe everyone has that ability...but it seems like I have an odd ability to move my soft palate open and closed just by thinking about it. For instance, sitting up in my computer chair right now...I can sort of control my soft palate and make it flap over and close the airway voluntarily. I'm wondering if purposefully doing that would strengthen some of the tissue in it that may have lost muscle mass over the years. On top of that, when I brush my teeth before bed...I tend to get a thick phlegm-like substance in my throat that forms because I guess the toothpaste irritates my throat or something. So I'm not sure if it is just some gunk that gets stuck in my throat and seems like apneas/hypopneas or like my throat closes over because it sticks the soft palate closed like a temporary glue.
Probably 2-3 weeks from now, I'll buy the Air Sense 10 and see what happens. On the nights when I do seem to sleep better due to sheer exhaustion, I have some pretty terrifying dreams. Starting to wonder if I'll have more of those when I get on the APAP. I've read that some people who get more REM sleep start having a lot of them when they get on the machine.
I guess at this point it doesn't so much matter what exactly is happening as long as I can identify and the machine helps. What I think happens is when I lay down and go into a deeper sleep stage, my soft pallet relaxes and becomes sort of flappy-like. As best as I can tell, I feel a little better when I sleep more on my stomach and turn my head to the side compared to just on my back. There have been a lot of times when I woke up and my brain was awake and alert enough to think it was my upper throat closing over and yet my body was still asleep and relaxed to the point where I could simply lay there and recreate it within seconds by letting my throat relax. At that point, it feels like the soft palate closes over my airway in what seems like a flap-like fashion. I'm not sure, maybe everyone has that ability...but it seems like I have an odd ability to move my soft palate open and closed just by thinking about it. For instance, sitting up in my computer chair right now...I can sort of control my soft palate and make it flap over and close the airway voluntarily.
I think that you may have some positional apnea because of your description above. I haven't seen any of your Sleepyhead charts so I can't look for any confirming evidence. The common way I explain it is that your chin is tucking. If you would try a loose fitting soft cervical collar (we do not want on the front of your throat, we are not trying to immobilize your neck, only to stop your chin from dropping. If I am right you should feel remarkably better.
Fred
If I am reading your Sleep Report correctly you spent the large majority of the night on your back (Supine), and most of your AHI and RDI is accounted for in that position. Next seems to be sleeping on your right side, and a somewhat proportionally lower part of the AHI and RDI comes from that position. I think that having more apnea when sleeping on your back is fairly normal. Your throat relaxes and your tongue goes back and you get a restriction or blockage.
Fred may be correct in that a cervical collar could help. At $10-15 they are much cheaper than an APAP. But other than from how you feel in the morning, I'm not sure how you could tell for sure it was working. But if you feel better, then perhaps it does not matter. You have your answer.
Possibly. They look a little uncomfortable to sleep with, but I could try. Would a soft collar work or is there a certain kind? I see that they use cervical collars to treat persistent apneas in people who are already on CPAP and still get apneas.
Definitely a soft collar. I have recommended it many times to use with a CPAP and most can visualize the difference on their SleepyHead charts by the loss of clusters with their Obstructive Apnea.
Top be clear I am not saying this is a cure or that this will replace a CPAP.
One question. Is your issue on inspiration or expiration? Expiration implies a different problem.
I like that the Dr. Dakota Snore Eliminator has a flat back compared to a regular cervical collar. The idea seems to be to keep the chin from pitching downwards and sort of reminds you and prevents it from happening when you're too tired to think about it while trying to sleep. I'll give it a try for the $15-$20 before I go for the APAP. I found a similar one like the Dr. Dakota one, but it is called The Eliminator Sleep Cushion and is basically the same thing with a flat back and strap and only the cushion part on the front to keep the chin from moving. It actually looks more comfortable in the photo compared to the Dr. Dakota one. For $12, it can't hurt to try that first.
It is unknown if my issue is with inspiration or expiration. I want to say inspiration, but sometimes it seems like both. It is like the soft palate (or maybe it is the adenoids, I don't know)...flaps over my airway both when breathing in and out when my throat is relaxed. I can make it do that partially when I'm sitting upright at any time of the day. Just not sure what it is exactly and the only option for that would be more surgery, which I don't want.
I believe flow limitation and apnea can happen on inspiration and expiration. That is why there is a benefit to turning off EPR and Flex on a PAP device. That prevents a reduction in pressure on the expiration.
You are correct, On another forum we had a user that had Palatal Prolapse with very similar symptoms but she was very specific about the issue being on exhale so I do not think it applies here. FYI here is a link to what the flow rate looks like with this. [http://www.apneaboard.com/wiki/index.php?title=Optimizing_therapy#Palatal_Prolapse]
So I tried the flat back cushion last night and it was terribly uncomfortable. I think I actually slept even worse because I kept waking up wondering what that was on my neck and trying to adjust it away. My neck hurt a little when I woke up. These things seem to be made for back sleepers only. Trying to sleep on your side or stomach is just one of those things that isn't happening very well. I wonder how typical that is? I also have a 4"-5" pillow that is rather stiff (called a Noffa pillow) and is basically a stiffer memory foam pillow that I bought a year or two ago to see if it would help my sleeping. I used to think that my pillow being too flat might have been causing obstruction of my airway. Now I'm thinking about going back to a little bit flatter and softer pillow. Still can't quite get used to that one. I would think that being too tall or too stiff could also have an adverse effect just like being not tall enough. It has me wondering if I'll feel this same way with CPAP.
I think some do it, but I find it hard to imagine how one would sleep on their stomach with a PAP mask. I guess having a pillow shaped like a toilet seat might work. Most I talk too sleep on their side and let the mask project out off the side of the pillow. Before PAP I used a memory foam orthopedic shaped pillow, but I found it was too stiff and pushed back too much on my mask. I now use a much softer down alternative pillow.
They have one like this that supposedly works for stomach, side and back sleepers using CPAP. Odd shape to it with a cutout on each side.
https://www.amazon.com/CPAP-Pillow-Adjustable-Height-Ergonomic/dp/B07DX7D2MC
One question. Is your issue on inspiration or expiration? Expiration implies a different problem.
I am getting over a pretty bad cold. I should note that when I have a cold and have to blow my nose rather hard, the air in my upper throat area abruptly halts as I'm blowing because it feels like a flap in my throat area closes over upon the heavy exhale. Not sure if that's just loose tissue and if it is also what is happening when I'm sleeping or what. Could be an extended soft palate, extra tissue on it or whatever. I feel like it is an extra flap somewhere.