Hi sleepydiane and welcome to the forum:
Yes...only I was able to keep up with school...I just couldn't seem to make it to the school bus on time. This was very vexing to my mom, because then, she would have to get up and drive me to school. I was often late. I was even late for school in England, as a 12-year-old when we lived there for a year. The schoolmaster didn't take kindly to this and I wound up in the headmistress' office. This wasn't fun. I still couldn't seem to get myself out of bed. When I did make it to school, I was always rumpled up and not quite awake yet. The schoolmasters thought I just didn't like school. Fortunately, enthusiasm was not a graded subject...
Hi - newly diagnosed hater of the CPAP LOL - I posted a question about how long to start feeling better - I have it pretty severe - 738 episodes in 7 hours of sleep during my sleep test - Oxygen saturation dipping to 77% at times - and minute and a half intervals where I completely stopped breathing. I have diligently used the CPAP since I got it, great results even though I hate the thing - but don't really feel better after 3 weeks. Here's to hoping!
Hell, my name is Oscar. I’ve been using a bipap for about 6 years, it has really changed my life for the better. I have mostly central sleep apnea and no matter how much weight I’ve lost I’ll still be on a bipap till death do us part. I was at least able to get the pressure lowered some, I’m currently on 16/12 setting.
Hi, my name is Karen and I am new to all of this. I was just diagnosed with OSA and have been using a CPAP machine since the August 23 2018. I am using the Phillips Respironics DreamStation with the AirFit P10 nasal pillows system. I really haven't seen much difference yet but I know I have just started on this journey and hopefully I will soon start seeing the difference soon. So open to any tips that you all may have.
Keep an eye on that P10. The P10 is notorious for the straps stretching and requiring frequent replacement.
It is true that that the AirFit P10 headgear is poor, the straps stretch, and the adjustment clips they give you are next to useless. That said it is easily the most comfortable mask of the 5 different ones I have tried. I now use a Breathewear Halo chin strap to both keep my mouth closed and keep the mask straps in place. I keep intending to cut the straps, overlap them and sew them back together again (to make them tighter). I'm at 6 months and still on the complete original mask.
Karen, what was your AHI at diagnosis, and what is it now? For what it is worth, I never noticed any immediate ah ha benefit. But, after 6 months I do think my sleep quality is significantly improved. My AHI has come down from about 34 to around 3.
Hi Sierra My AHI is 19.4 events per hour and 30.2 during a 3 hr and 2 minute events, oxygen saturation is 95% baseline and 83% lowest so the average came to 91. I was told that I have moderate to severe OSA. So far the p10 is working. My problem is over a month in to using the cpap machine and I wake up tired, no energy and still have daytime hypersomnia. I am getting very frustrated. I haven't checked to see what my AHI is now. I am so new to all of this where do i find my readings now? Any help would be greatly appericated.
Hi All, I'm new here, in the U.K., 57 years old, of average build, and have recently started using a Philips Dreamstation CPAP. 'Recently' meaning I've had 9 nights with it. My sleep study AHI was 19, and according to Philips it's now down to around 1.5. I'm assuming that the AHI figures from the study are directly comparable to the device. If not, then how do you compare them? Not sure yet whether it's my imagination or not but the feeling first thing in the morning of doing a round or two with heavyweight boxer seems to be receding! Which has got to be good. Throughout the day, too I'm not feeling quite so wiped out, and I've restarted the gym visits. Eventually, I'd like to get back to cycling and doing 50-60 mile rides which seem a lifetime since. Regards, MTD.
Welcome to the forum. Yes the AHI reported by your machine is reasonably comparable to a sleep study. If you want to look at your results in more detail I would suggest downloading SleepyHead. It is free software made to display and track your detailed data from the SD card in the CPAP. You will need a SD card reader to transfer the data from the card to your computer (Apple or PC).
The AHI reported by your machine is designed to err on the side of overestimation, so it may be a little higher than that from a sleep study. This is not unusual amongst medical devices, as a false positive, resulting in further investigation and eventually finding out that everything is OK, is more desirable than completely missing a problem altogether. Also, there are various things which can trick the machine and lead to a much higher AHI being reported than is actually the case (Periodic Limb Movement Disorder is a classic case in point). So, the AHI from your machine can often be a little higher, and sometimes a lot higher, than you would get from a full sleep study, but it will almost never be lower. SO when you get nice low numbers like an AHI of 1.5 you can be pretty confident that you are doing very well.
Hello,
I am a 73 yr old male with OSA noted to be highly REM associated and moderately severe. Determined by a Polysomnography in 2000. I am presently using a Dreamstation APAP which does fine. My problems: Frequent power failures, Airlines losing bag requiring me to carry on Machine, Not convenient to use in flight. Not available when visiting friends and I want to Nap.
I have just completed a consultation with a local Dentist who specializes in Oral Device Herbst device. Since I have moderately severe OSA would you feel I could have a reasonable expectation that this would be a good alternative to APAP when not available in the above mentioned circumstances?
I have read when oral devices are effective in light to moderate OSA. Would you advise me that it would be counterproductive and too expensive to go ahead with this additional option?
I would be so appreciative if you could give me some help and advice re this issue.
Best Regards,
Ronald Pogatchnik rpogatchnik@gmail.com
I can' really comment on your specific situation for 2 reasons 1) I don't have the data required to understand the situation properly and 2) I'm not a doctor (I'm a tech). Also, I am in Australia, and I know that the cost of various treatments is very different in other countries. All I can say is that among the many patients I have seen the success rate with oral devices is quite low and they have all been very expensive. That doesn't mean it won;t work for you though. Look into it thoroughly.
With regard to your portability problem, it is possible to pick up travel CPAPs which are quite small. One of these may be helpful for travel. Have a look on https://www.secondwindcpap.com to get an idea of price, and google some pictures for size. You can also pick up batteries which are not too big and will run your CPAP for 8 hours or so at a time.
Hello, my name is Adam. I was diagnosed with OSA about 2 weeks ago. So far my CPAP has seemed to help a little so far. Although I know it could take a couple months to feel the full effect of it. I have the Resmed 10 Auto and my pressure is adjusted to range from 10 to 20 as I am sleeping.
Welcome Adam. The ResMed A10 AutoSet is a good machine. You may find that after a while you might want to tighten up the minimum and maximum pressures some. As I suggested to Max in the previous post, you may want to download SleepyHead so you can see what the machine is really doing during the night. I have the same machine and started out with a wide range like that. Now I am at a minimum of 11.4 cm and a maximum of 12.6. If you need any help just post your questions in a new thread.
The cpap is working good for sleep apnea. However, I seem to ha e recurring corneal irritation since starting to use it. I’m wondering about the pressure causing dryness to the eyes & whether that could cause my eye issues. I need to have cataract surgery but cannot seem to get my cornea healthy enough. The corneal eye issues began after starting cpap therapy. Does anyone else have eye issues?
I found that with certain masks, I had air leaks into my eyes. Although my eyes were shut; it was still most irritating. Could you have a mask that is leaking into your eyes? These leaks are kind of small compared to whole mask leaks. What type mask are you using? You shouldn't be getting dryness in your eyes as a result of therapy unless the mask is a problem to my thinking but I am just another patient.
When I was using a full nose and mouth mask I was plagued with mask leaks near the bridge of my nose. The air leaks irritated and dried my eyes out. And it would also wake me up. I have given up for now on the full face mask and gone back to a nasal cushion mask. It still does leak occasionally, but at least the leaks don't go into my eyes.
Hello, I’m new here. I just had the CPAP portion of my sleep study last night. I can tell that my head is clearer today, from the moment I woke up; They actually let me sleep until 07:00am.
I watch for people’s POSITIVE CPAP experiences, because the negative stories will only add to any hesitation to do what I need.
I used a nasal pillow type of thing that’s just had a hole where it pressed against my nares. The air connection was on the top of my head. This is SO MUCH EASIER that full face or nose “masks!” I didn’t sense ANY phobias about difficulty breathing. It just takes a bit of getting used to.
I’m looking forward to receiving my machine and feeling more alert, with fewer body aches, on a daily basis. My mom (and my ex-husband) had CPAP, and I feel really blessed that there are new types of gear which makes using it so much easier.
I don’t want to be literally dying every night, for lack of oxygen, and I want mental clarity every day! Yeah, aches and pains from sleep deprivation will diminish!!
So looking forward to the benefits of HEALTHY SLEEP!
Hello everyone, I am 33yrs old (m) and recently diagnosed with a home study device for mild mixed sleep apnea. As you see from my first thread (https://myapnea.org/forum/need-your-feedback-how-to-set-expectations-deal-with-central-sleep-apnea-diagnosis-as-part-of-mixed-sleep-apnea), I am right now dealing with the potential implications/causes for the central sleep apnea part, which scares the hell out of me.
I am the guy who panics and draws the worst conclusion. Especially when the doctor drops words like "your brain forgets to breathe", I am already thinking of tumors or other neurological illnesses since I am not taking opioids and never had a stroke.
Hello,
My name is Chris. I'm 34 and just got diagnosed via a sleep study for sleep apnea (68 events per hour and got down to 70% on the oxygen level). Oddily, don't feel too tired during the day, but I might have gotten used to a lower energy level and made adjustments to compensate. Anyways, tonight will be the first attempt with a cpap machine. Resmed Air sense 10 etc.
Welcome to the club that nobody really wants to belong to! Good luck with your cpap machine tonight. The first night can be a little difficult to sleep with everything new that is going on. What I can suggest is to do your best to relax and try to get some sleep. You may want to plan to use it while watching TV or reading before you actually try to sleep with it. I use the same machine as you have and it is very good. If you have any questions about it just ask.
Greetings folks. Im a 58 year old male. I have Afib and now diagnosed with severe OSA. I am waiting patiently for a machine. I did the split night study, and found the CPAP atrocious and amazing. The mask was uncomfortable and caused some side effects. However even with that I got some of the best sleep in years for a few hours. I feel confident i will find a better mask and maybe an adjustment in humidity will help with dryness. I actually had blood from dryness from throat. I did mention it halfway through test about dryness. She was going to adjust humidity. Could be damage was done. One thing for certain is I can not continue to live like I am. My body fights all night long. Sleep comes in minutes or even seconds. I keep my wife up by huffing and puffing. My days are tired. If you are the praying type, I would ask you might say a little prayer for me. I am over 2 months into this. Waiting for someone to contact me about a machine. Tonight I will suffer again, hoping the Lord will wake me for tomorrow. I am optimistic. I worry I waited to long before seeking help. <sigh>
Hang in there. If you can I would suggest a ResMed AirSense 10 AutoSet for a machine. Also it would be nice to have a heated hose (Climateline) to ensure you get the right humidity to stay comfortable. Masks are tough. Everyone seems to like something different. About all I can suggest is to try more than one style if that is possible.
Hello there, my name is Eric and I’m 37 years old. I was diagnosed with mild sleep apnea a little over a year ago due to the extreme daytime sleepiness that I’ve lived with for almost a decade. Couldn’t afford to do anything about it, but this year I found that I couldn’t get life insurance, so I was forced to do something due to the diagnosis.
The sleep study this year showed the same AHI as the last one at 6.8, which are mostly hypopnea events. The thing that prompted my going for a study last year was my wife waking me when I stopped breathing as I fell asleep (I stop breathing for ~20s as I fall asleep, apparently, which I didn’t know until she noticed and started waking me when I did it).
This year I have insurance that covers things, including a CPAP. The sleep medicine clinic set me up with an Airsense 10 Autoset and bet on a mirage fx nasal mask working best for me.
As of today, I’ve been using it for four nights. It always gives me a score of 100, which worries me. The worst leaks were with the full face mask and the least I’ve attained was with the nasal mask (claimed no leaking at all last night); my best AHI thus far was last night at 0.5. The FFM also was less comfortable from the air blowing all over my face.
My biggest problem is that it starts pulsing as I fall asleep since I stop breathing as mentioned above, which makes it harder to fall asleep. Beyond that, the first night I felt bloated, but that has gone away. I still have chest and upper back aches all day... On the upside, after the first night I wasn’t yawning all day.
Is it normal that it seems to cause you to lose your appetite? Since starting, I’ve been skipping one meal a day and eating less in general.
If you have a PC or Mac with a SD card reader, you may want to consider downloading SleepyHead to get a more detailed account of your machine performance. The software is free. Here are a couple of links:
This software will graph your mask leakage throughout the night and give you a more accurate reading of actual leakage.
As for masks I have tried two full face models, Mirage Quattro and AirFit F20, but did not like either one. They leaked too much for me and blew air in my eyes which kept me awake. I tried the Mirage FX nasal mask, but found it a little restrictive. I couldn't scratch my nose when it got itchy at night! I started with a AirFit P10 nasal pillow mask, and have also tried the F&P Brevida model as well. But, after all of that, I am back to the P10, and like it the best. That said each mask is a personal experience and not everyone likes the same masks. About all I can suggest is take opportunities to try different ones.
How much data does it collect each night? I would love to see what it actually shows. Last night it claimed 0L/min, which sounds strange since I ran the mask the loosest I’ve ever run it.
I like that the mirage allows me to adjust the angle with the upper straps so it stopped blowing in my eyes. The full face mask didn’t blow in my eyes, but the machine said it lost the most air. It also has a different attachment piece that lets a lot of air out, so I’m wondering if that caused the difference in readings.
I’ll have to try some more. I remember finding the nasal pillow mask being quite uncomfortable when they tested one on me during my first sleep study. That said, they do look less intrusive and if I could get my nostrils used to them, they might work. Will have to see what options I have there.
Assuming you have a SD card in the machine, it should have all your data from day 1. It will show from minute to minute what your actual leakage is. I will post an example in response to your post above so it will display wider.
My wife has switched from the Mirage FX to the F&P Brevida (the one I didn't like so much). These nasal pillow masks usually come with a fit pack of the different sizes of mask inserts. If you use one that is too small it can go too far into the nose and cause irritation. Too large and they don't usually seal so well. If they fit right, they should be very comfortable.
The weak part of the P10 mask is the headgear. There is an older ResMed Swift FX nasal pillow mask that is quite similar to the P10 but has a better headgear setup. It may not be quite as compact though.
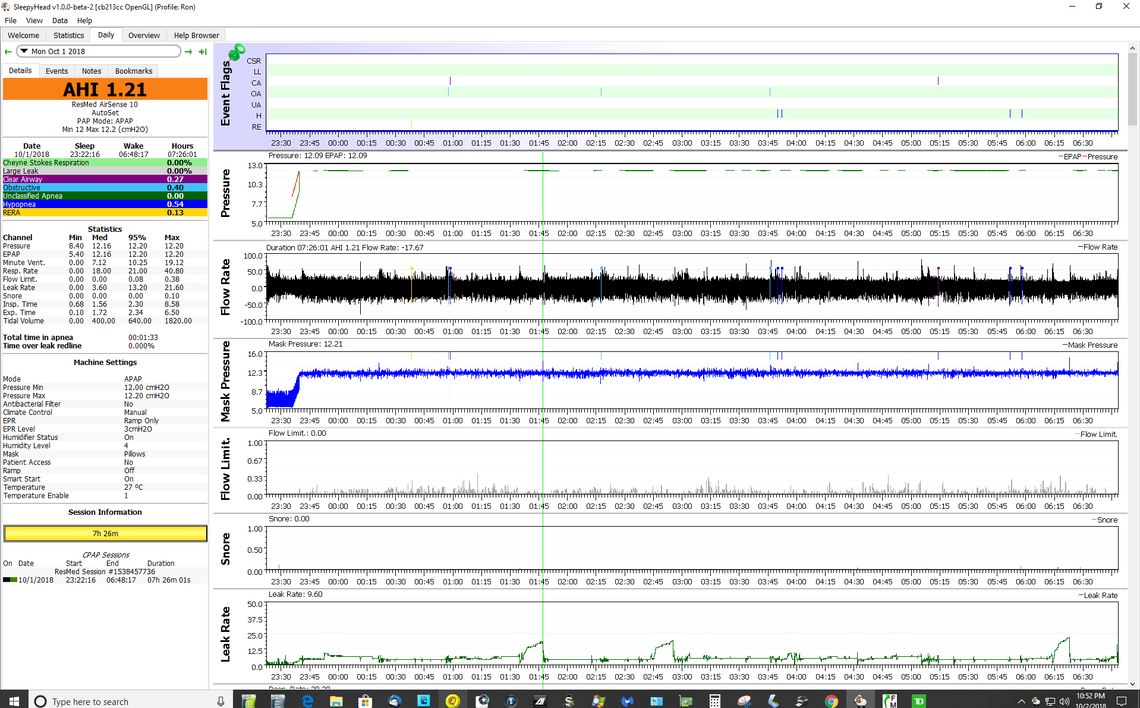
Here is an example from my sleep report from a few nights ago. This is with the P10 mask. This is shown at full scale for the screen capture, but when you use the software the up down arrow or by left clicking you can zoom in to see a breath by breath response. The amount of data and the detail is amazing. There are more variables by scrolling further down, but I put the ones I think are most important at the top.
You can see that I had three periods of higher leakage, but in total I had zero time over the leak redline.
Hello all! This is the first time I've visited this forum. I'm new to the forum but not to CPAP. I am likely the dinosaur around here. I've been using CPAP continuously since 1992. That's right, more than 25 years. Back then no one had heard of CPAP and even most doctors didn't know what sleep apnea was. My first sleep study recorded 66 apneas per hour. CPAP absolutely transformed my life. I had been having such severe memory problems that it became difficult for me to work. At the time there, of course, was no support group and almost no literature about sleep apnea or its effects. Even the technician that brought me my first machine knew next to nothing. He told me that I should be careful because the machine could cause me to "blow a lung". I now know that was a stupid thing to say, but I too was ignorant, as well as confused and a bit scared.
Hi, I’m Bill. 58 years old. A long time sufferer with no treatment. I gave up on CPAP very shortly after I was diagnosed 15 years ago. My life has gotten unmanageable. Always beyond exhausted. Finally I learned about Bipap and researched it. I experimented without going through a doctor so I’m not sure what my current HCI without treatment is, but I’m sure it’s severe. I’m on my fourth mask I think I’m about to figure it out. I’m using a ResMed N20 nasal mask and the best I’ve been able to do is a 10 HCI with it. I have ordered a large nasal piece to replace the medium and I think that’s gonna do the trick. I hope so. After i succeed on that for a few weeks I’m going to tell my doctor all about it. I actually got an old bipap on line for cheap because I didn’t want to pay for another sleep study before I knew if I could tolerate a bipap. No insurance. I replaced the cheap bipap with a Dreamstation auto bipap. After 3 months I think I’m about to figure it out.
Bill, This sleep apnea stuff can get expensive without insurance. A titration study would pinpoint the settings needed for you to have meaningful therapy. NO one here can help you decide which type PAP machine is best nor the pressure(s) needed to control your apnea. I suggest you save up and do this thing right by paying for an in-lab study if at all possible.
Hi Bill. Welcome to the forum. It is good to hear that you are giving CPAP treatment a second chance.
The DreamStation Auto BiPAP is a very good machine, but is fairly complex to set up properly. Do you have a manual for it? If not here is one you can download from this link:
I would recommend as a next step if you have not already done so to download SleepyHead so you can view your detailed sleep reports. The software is free, but you need a PC or Mac and a SD card reader to use it. A couple of links:
If you want some help with getting the machine working for you, it probably would be best to start a new thread as posts tend to get lost in this Introductory thread. But, if you give some details on how your machine is set up, what pressures you are running, and what the breakdown of your AHI is. The key part at this point is the ratio of obstructive apneas to central apneas. A good way to communicate this is by posting screen shots of your Daily Report in SleepyHead.
Hi,
It's me, or at least I think so. :P
I didn't intend to kill this thread too! :(
I live in Australia and have very severe OSA
I have a Resmed 9 which I detest!
This is the first time I have involved myself in any forum for a very long time.
My wife has the ResMed S9 and I have the newer A10. I think both are basically good machines, but the A10 does have a few advantages, and possibly one disadvantage. First with the disadvantage, I normally stand up to change the setup or check the data on my machine. I find the top display and controls on the S9 more convenient. My wife also likes the lower profile of the S9 because she can put it in the night table drawer and close it when not in use.
The advantages of the A10 are that it overall is smaller and a bit easier to travel with. The case has a loop to attach it to a travel bag that the S9 lacks. The data storage capability of the A10 is much better. The S9 only stores a limited amount of data and then starts to write over the old data. The A10 can hold months of data before it starts to overwrite. So, if you are a SleepyHead user you can slack off on transferring the data to your PC, without losing any data. But, the biggest advantage of the A10 is the Auto Ramp feature. While both the S9 and A10 can be set up to use EPR on ramp only (which is my preference), only the A10 has the auto ramp feature which goes to treatment mode when it detects you are asleep. I think that is far superior to the gradual ramp of the S9 or other machines, if you do have trouble going to sleep wearing this contraption. The gradual ramp up starts with a lower pressure and constantly increases it until it times out. Especially if you are a new or anxious user you can start thinking "I better get to sleep or the pressure is going to get too high and I will never sleep". The Auto Ramp is not really a ramp, but a pressure hold. It keeps the pressure constant until it detects you are asleep. It times out after 30 minutes, and goes to treatment mode, but I find I most often go to sleep in 10-20 minutes and I don't get to that point.
My last thought is that I think the Australians (ResMed) are ahead of the Americans (Phillips - DreamStation) when it comes to CPAPs. The unfortunate part is that the ResMed machines apparently are much cheaper in the US than in Australia (in $US). And they are even cheaper still in Canada. Why? Must be a government duty or tax thing, or a company strategy. Don't know. Now if you are thinking about upgrading your machine and are not in a hurry, keep in mind that ResMed is getting to the point where it is somewhat overdue to release a new model. Could happen anytime. I think the next major breakthrough in CPAP technology is the use of AI. It may be a little early to see that in commercial form though...
Hi Sierra,
Thanks for so much useful information. I don't know how you have the patience to deal with people the way you do.
Firstly: Of course the Australians are ahead of the Americans! Isn't that always the case? :O
Secondly I don't use the ramp because I need to breathe right now not just when it gets around to it!
As to comparative machines ........... Unfortunately my detest has no prejudices. I detest the Resmed 9 as well as the Phillips machine I used while it was being serviced, and I also detest the F&P Icon that I bought to leave in the car boot for unplanned stop-overs.
It well might be that I simply detest being shackled to a machine? :P
If I should ever manage to mend my attitude the Resmed 10 does seem like a nice machine but I would probably have to buy it out of my "special treats for bribing grandchildren" fund because I doubt that the hospital that supplied the machine would upgrade this one unless it died of natural causes and even then I think they have switched over to the Philips machine which I detest even more vehemently than the Resmed.
As to invoking AI the very thought is disturbing! Like we haven't got enough interface problems when the machine has only a limited range of settings and outcomes and STAYS PUT where we set it!
I can see some situations where it might be invaluable and even life saving but I doubt that it would pan out that way for everybody.