For around two years now, I have been suffering from some kind of sleeping disorder which is making my life very difficult.
There is some kind of fluctuation/irregularity in my breathing rhythm that causes me to wake up exactly at the point of falling asleep. It can go on all night sometimes and, unless I take sleeping pills, happens every single night, and has done apart from a four-month period from Feb 2017 - June 2017.
I'm a life-long asthma and allergic rhinitis sufferer and therefore thought the problem must be related to this. I went to see a pulmonologist in September last year who gave me some inhalers to treat pulmonary obstruction. Several weeks later this hadn't worked so I had a sleep test. Based on the results, I bought a CPAP in December last year, which I feel helps a bit and generally makes it easier for me to breathe when I'm lying down, but doesn't really address the problem.
After 3 months of using the CPAP and not noticing any improvement, I decided that maybe the cause was neurological rather than pulmonary and went to see a neurologist with a specialisation in sleep disorders and had a sleep test sometime after. The results came back negative, there were no central sleep apneas according to this test, despite the fact that during the sleep test I had experienced these same problems. The doctor told me that the test could only measure apneas of at least 3-4 seconds, and mine are sometimes just a second or two long, at the exact moment of falling asleep, which may explain that.
I then decided to explore the possibility that it may be stress/anxiety related, despite the fact that I wasn't feeling particularly stressed or anxious, at least as far ad I was aware. I took sertraline for 5 weeks and noticed no difference in either my breathing problems at night or my mood and decided to discontinue it, gradually. I no longer use it and feel the same as when I did. I also went for hypnotherapy sessions, which I found very relaxing but didn't have any effect on my breathing problems. I also tried, and still do, breathing and relaxation exercises before bed, which again are very relaxing but do not make a difference to my breathing problems.
I decided to go back to exploring the possibility that it was physical rather than neurological or emotional, and saw two ear-nose-and-throat doctors, both of whom recommended having a septoplasty to correct my slightly deviated septum. I had the surgery on September 13th. The operation was a complete success and has almost fully healed, yet here I am at 3.35 in the morning (I'm in Mexico) unable to get to sleep due to this strange change in my breathing that occurs at the moment I fall asleep. I have done a lot of research online, and can find a couple of references to something called "transitional sleep apnea" or "sleep-onset apnea," which seems to kinda describe what I'm going through, but sadly doesn't seem to be a common occurrence and there's to be little known about it, let alone a consensus on what causes it or how to treat it.
About 6 months ago, I thought there was no way I could possibly carry on this way, but the problems have persisted and I simply don't have any choice but to carry on. Sleep deprivation is now the norm for me and the only way I can get to sleep at night is to take meds which make me fall asleep fast enough so that these events don't wake me up. These kind of meds, which I do my best to avoid, affect my mood, my memory and my concentration. I'm making mistakes at work and finding it difficult to remember things. I'm irritable. Most of all, I'm sick to death of this.
My next plan of action is to have cranial therapy. I have had one session already and again found it relaxing and am feeling (or trying to) feel optimistic that this may be of some benefit. Apparently, I have some issues with the bone structure in my head, probably due to some injuries that I received to my head when I was younger and the trauma from them. Also, according to this therapist, "energy" is not flowing up to my head like it is apparently supposed to. After having tried almost everything, I'm open to anything. If this doesn't prove to be of any use, I honestly can't think what to do.
Can anyone be of any help?
Thanks,
Joe
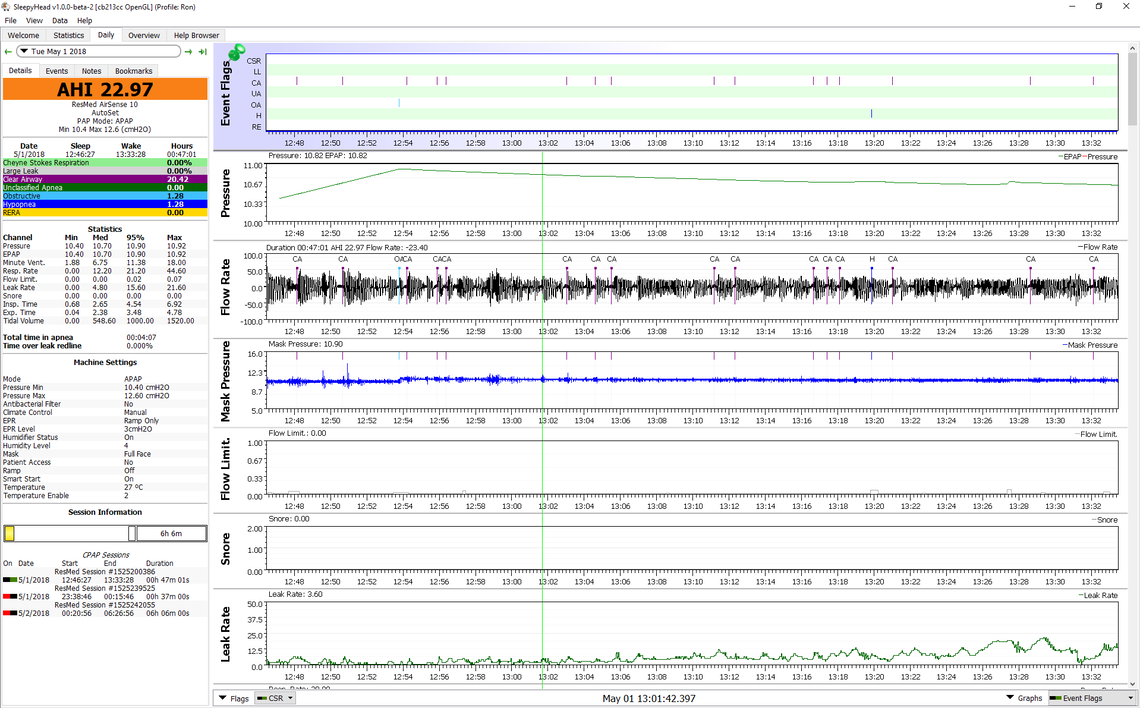
Joe from time to time I have had issues going to sleep. However for me it seems to be associated with my CPAP equipment. When I first started using a CPAP or try a new mask that doesn't get along with me, I can have issues. Here is one such event captured in SleepyHead which is a free software that one can use to display CPAP machine data. This was an attempted 45 minute afternoon nap to test out a mask that did not work well for me. I doubt I was asleep for much if any of the time displayed. However the machine recorded many CA or central apnea events, possibly as I went to sleep briefly and woke up again. This was using a constant pressure at machine start up.
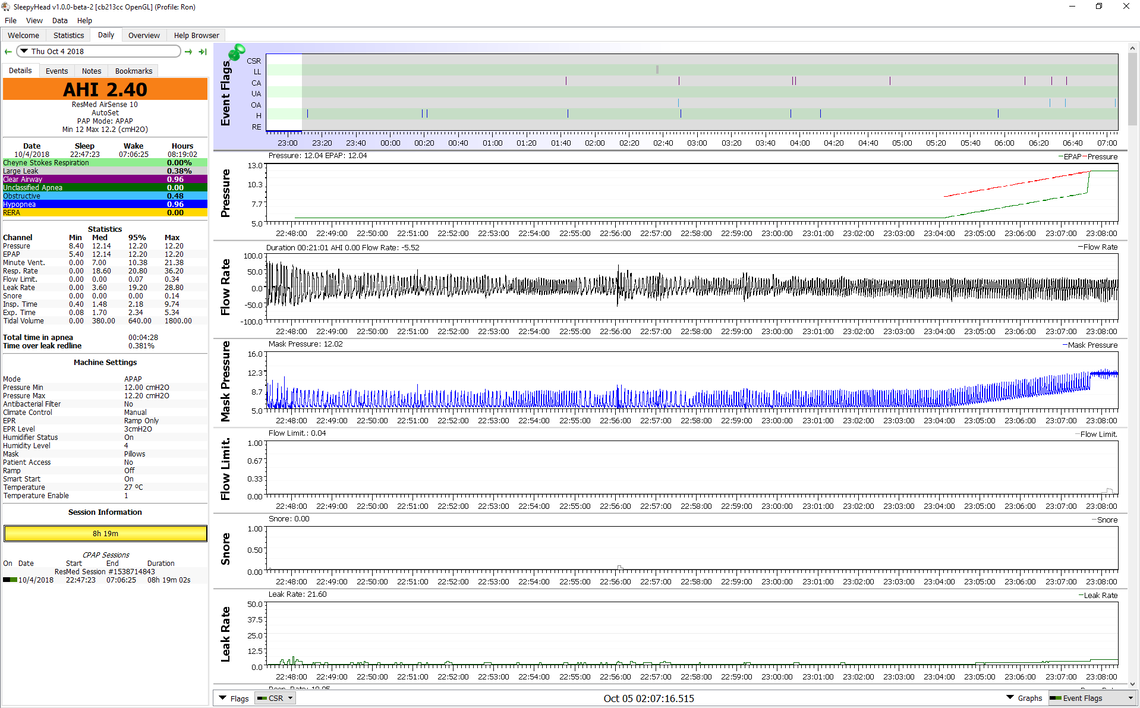
Now here is last night's going to sleep period where I am using the Auto Ramp feature of the ResMed AirSense 10. I also am using an EPR of 3, which turns off once the ramp/hold period is over. Notice that the breathing pattern is much smoother and no apparent apenea events. However they would not be flagged, as ResMed suppresses the report during the hold/ramp period. I think the other part of this is the EPR function where the exhale pressure is 3 cm lower than the inhale pressure. This may assist breathing and avoid some of the sleep wake irregular breathing issues. Notice that at some point the breathing becomes quite regular (probably asleep), then the pressure starts to ramp up, and when it reaches set pressure the EPR stops, and the mask pressure stops cycling up and down.
If your machine is compatible with SleepyHead you may want to use it to look at your areas of difficulty and see in more detail what is going on.
Wow, thanks so much. I have the ResMed bu6t have never heard of Sleepy Head. Do you take this info to your doctor to be analysed? While I definitely think that this data may turn out to be useful in trying to figure out what the problem is, I don´t think the problem is the CPAP itself. I have had these problems for over a year before getting the CPAP and in fact, things have been slightly better since starting using it. But I´ll look into this and see if y machine is compatible with Sleepy Head. Also, I don´t my apnea events will be flagged either, as they are so brief (I don´t use a ramp) but maybe this could shed some light on what is going on with my breathing patterns during the transition to sleep.
Thanks for your input.
No, I did not take the data to my doctor. I just concluded that this full face mask (Mirage Quattro) was not the one for me. For what it is worth, I don't think these events flagged by ResMed as central apnea events are real apnea events. It is just the waking up and going to sleep process. Some call it sleep wake junk. And that is kind of what it is - Junk. That said if it is happening all the time it is not going to be helpful in going to sleep.
If your machine is a ResMed like the AirSense 10 AutoSet it certainly is supported by SleepyHead. The older S9 model is too. To run SleepyHead you need a PC or Mac with a SD card reader. Assuming your ResMed has an SD card in it, all the data will be on it, so you can go back and look at it.
How do you have your CPAP set up to go to sleep? Do you use the Auto Ramp? EPR On? EPR Full Time, or Ramp Only? These are the features that may help you get over this going to sleep apnea issues.
I now see you are not using the ramp feature, so the data you have collected should show all of what is happening. But, once you see what is going on, then you may want to set the ramp features. It is far from a sure thing to help you, but worth a try. It should improve the comfort level. If you need any help just identify your specific model of ResMed and I may be able to answer your questions. And while the machine may not flag the apnea events, you will still be able to zoom in and look at your actual flow rates to manually identify a stoppage in breathing, even if it is only for a few seconds. All you do is left click on the area of interest. With each click it zooms in further until you can see every breath.
Hi Joe. Maybe it will help you to know someone else has the exact same problem. Me. I have been trying to figure out what is wrong with me for a yr now to no avail. Googling and googling....until tonight I found your post!!!!
It is 4:17 am and I am giving up even trying to go to sleep.
I too am coasting on 3 hrs sleep/night and this has been going on for a year now every single night every time I start to drift off to sleep. I have no problems going to sleep and I am not stressed at all.
The sleep study I had done showed I have moderate to severe obstructive sleep apnea, and I also have a deviated septum like you. I tried the CPAP for a couple weeks and it seemed to be starting to help until I woke up choking....they said the CPAP was blowing air into my esophagus vs my airways. My dr is checking with the sleep specialist to see if reducing the pressure will help. But, just like you, even with the CPAP on....it still happens.
The way you describe what is happening to you is bang on how I would describe what is happening to me with one exception you did not describe. When I wake up only after 2-3 minutes, I have this scary feeling/sensation, which I think is the experience of stopping breathing. Do you have that too or do you just simply wake up? Last week I drove to the hospital emerg at 5am out of sheer desperation (I avoid hospitals at all costs).
I guess I also wanted to rule out it being a heart problem because of that feeling of dread I described when it happens. Hospital said my heart was fine, blood work fine too but hooked me up to a heart monitor and sent me home to track my heart for 48 hrs. Results came back fine (I had to keep a diary/log and write down the time these events I described were happening while I was wearing the monitor. My family Dr. compared those times to the heart rythm report and results were fine. Whatever this is must be uncommon because my Dr isnt sure what to do next and it took me a yr of researching sleep disorders myself online until I found your post. I am going to keep trying to figure this out simply because I just want to be able to sleep once again and dont want to take pills. If you find out anything else in the meantime I would be very interested to know what you do find out.
Thanks for any light you can shed. It does make me feel a tad better knowing someone else is going through this!
Darlene
Hi Darlene, thanks for your message.
I'm very sorry to hear that this is also happening to you, I know from first-hand experience how demoralising and upsetting this problem is. I also have spent a lot of time researching this online and finding little information, and none of the doctors I have seen know what to do either. I'm setting in to relax for the evening so I 'm only gonna write a short response here, but in response to your question, no, I don't have that sensation of panic or dread when this happens to me, I remain very calm. I get super angry and frustrated sometimes, but nothing like you've described.
If you'd be ok with it, I wonder f you'd be interested in exchanging email addresses or phone numbers so we can share any potentially useful information? (this goes for anyone else reading this who is suffering from the same problem)
Best, Joe
Hi Joe, I found your post to be such an accurate description of what I am experiencing, today, I actually asked my family Dr to read it off my iPad and he did!
(I always feel rushed when I try to explain it to him because he is so busy). He seemed to get it after reading your post and also better understood how badly it is affecting me. He is taking it more seriously so that is good. I dont plan to post on here anymore...I only joined to see your post after it came up on a google search when I was trying to figure out what could be causing my symptoms.
I dont really want to put my email on here because its my full name but if you are ok with putting your email on here, I can then contact you just so we can update each other if we learn anything significant that sheds light on this problem and/or a solution that doesn’t involve tranquilizers.....which I declined when suggested today.
Thanks Joe
Darlene
Just out of curosity. Since I have sleep onset apnea as well, have you considered BiPap or ASV machines with backup rate feature? It seems these machines can deliver a breath or two in a a set period of time if some are missing. Not sure if they work with Onset CSAs though
Hi. not sure if you are asking me or joe this question but if me, the respirologist did mention BiPap because the cpap is almost too strong for me on the exhale. I sure hope I dont need a ASV. That is a ventillator right? The thought of that sounds kinda scary to me. I havent heard of APAP....will have to look that up. Thanks for the reply
ASV is no more a ventilator than BiPAP. ASV is a sub-set of BiPAP specifically designed to treat central apnoeas (generally Cheyne-Stokes) in the setting of low CO2. This was something which conventional BiPAP was not always very good at. However, you should not be using either BiPAP or ASV unless you have conditions they were designed to treat.
What is wrong with using BIPAP specifically? It is similar to CPAP, except can deliver more pressure on inspiration to get past blockages. BIPAP won't force a breath. If you don't breathe, it does nothing. It just marks it as a Central Apnea. That is the way my sleep doctor described it. Now...ASV is totally different, in that it will force you to breathe. ASV shouldnt be used in people with certain heart conditions. You need to have your heart ejection fraction checked, before starting ASV.
But going back to the original post, I had the same onset apneas happen to me a few months ago. My doctors couldn't figure it out. I kept laying down at night, felt jittery/anxious, would fall asleep and immediately wake up, and felt like I wasn't breathing. My BIPAP kept showing CA's occur, which is abnormal for me. I bought a Contec SpO2 monitor to wear overnight, and it showed my oxygen dropping to the low 80's% during each event. I couldn't get any sleep since every time I tried to go to sleep, I'd immediately wake up and felt like I was stopping breathing at night. I'd go a night without sleep. Then the next night was somewhat okay again. But then the cycle kept repeating occassionally. Then a few weeks later, I was hospitalized for DVT/PE blood clots. During in the hospital stay, they put me on a oxygen monitor, and it also showed my levels dropping, whenever I would fall asleep. Yet the doctor didn't seem to care. They just gave me a sleeping pill that night, that really didnt work well.
But now for a few months again, I've been fine. There was only one or two nights where I had this anxious/panic feeling, and tried going to bed and had those same feelings where i was stopping breathing immediately upon falling asleep. VERY WEIRD! My doctor said to either just take melatonin or a half tablet of Klonopin before bed. Which is what I do now, and now I can sleep so far. I hope the issue never comes back. Because I saw many different doctors....neurologists, etc, and they had no answers and blamed it all on anxiety. I just don't see how anxiety could cause Central Apneas and stopping breathing at night though?
I do wish I could get a BIPAP with backup rate though at least, just to have that extra "security" that it would try to make me breathe, whenever i do have Central's. But my sleep doctor keeps saying I don't need it, and that the "backup rate" style machines are old style, and not auto-adjusting. He said if I would have a ton of centrals then I would need ASV.
I believe ResMed designates the backup function as the S mode. I also believe it is just a fixed 10 bpm rate. It does sound a little crude. This is available as an optional mode on the AirCurve VAuto, which does the Auto BiLevel as well. The AirCurve ASV is a much more sophisticated machine that locks on your breath pattern, and tries to restore (force) breathing on a breath by breath basis. In Canada the VAuto can be had for about $1200, while the ASV is close to $5000.
Your sleep doctor is wrong. BiPAP most certainly can initiate breaths when set appropriately. You just need to know what you are doing. It is also incorrect to to say that BiPAP "is similar to CPAP, except can deliver more pressure on inspiration to get past blockages". It is not the inspiratory pressure, but the expiratory pressure which prevents blockage in your upper airway. The increased pressure on inspiration is to increase the volume of air which you inhale. To summarise:
CPAP is used to treat upper airway obstruction (OSA)
BiPAP is quite different it is used to treat respiratory failure and hypoventilation by increasing the volume of air you breathe in and out. It can also prevent obstruction at the same time. It is used to treat central apnoea when CO2 is not too low.
ASV is not used to ventilate the patient. It is used for treating central apnoea when extra ventilation is NOT required, i.e. when the patient is having central events but their oxygen and CO2 levels are otherwise OK.
I have the AirCurve 10 vAuto. This "Bi-Level" machine has no way to initiate breaths, even in it's static S-mode. ResMed has other models "AirCurve ST" and "ST-A" that have backup rates.
With the vAuto, if you quit breathing, the machine does nothing. It waits until it detects you are inhaling again. Even in static pressure mode it does nothing to force you to breathe.
Look up the specs on RedMed site for the standard "vAuto" machine. It has no backup rate and no function to keep your breathing if you have central apneas.
Perhaps I am not reading it correctly but the manual at the link below seems to suggest that the VAuto machine can be put in a "S" mode, and when in the S mode there is an optional Backup Rate which can be set to Off or 10 BPM. See page 14 in the manual at the link below.
Thanks for that explanation. Are you actually a sleep tech? Im trying to figure out what to do next. The sleep onset problem didn't happen at the lab during my sleep study because back then it wasnt happening every night like it is now. It was the reason for having a sleep study done though I also told the sleep dr, the respirologist, family Dr, emerge dr and now Im on here telling a whole bunch of people I dont even know too which is so not like me. Im very desperate for answers.
It seems nobody in the medical profession is worried about this and that is what I dont get. I definitely have some kind of sleep onset/sleep disordered breathing problem. This is such a scary feeling to experience every night multiple times. It is comforting to read both Charming coyote and warped trekker’s posts...both are very true to what I am experiencing. Why is the answer pop a tranquiliser to mask it so you just dont feel whats happening? When oxygen levels are so low isnt it possible you might not wake up to breathe at some point? I personally like living!!! if I cant handle CPAP due to my anatomy and CPAP wasn't stopping these events anyway, then what?
How do I confirm what this is and get rid of it? I dont want to just mask it and drug myself in order to sleep. I want to be able to function, have a clear head, earn a living and not die in my sleep!
Surely there is someone educated in this who can help, isnt there?
Who can best answer these questions?
Hello hello hello....is there anybody out there 🎵
Darlene, I am not a doctor, or sleep specialist, just another sleep apnea sufferer. Your post is kind of buried in the middle of another long thread. My suggestion would be to repost your issues from the beginning in a new thread. Include some details such as how long ago you did the sleep study and if it was an at home test or in lab test.
Yes, I am a real sleep tech.
Dang, the whole time I thought you were a professional rugby player! BTW: There is seldom much hope that replying to a 12 day old question will be seen by the person who posed the question! I really DO want to thank you for your participation as this forum lacks foundational professional insight and we get enough amateur babbling (like mine) already!
I just wanted to say a big thank you to everyone who has replied, and the info about the CPAP settings etc., is very useful. I'm gonna look into it for sure, but as these problems pre-date my getting a CPAP, I don't think the way the CPAP is set up is going to be the cause of the problem, although there is every chance reconfiguring the settings could lead to improvements.
I'll try and respond properly to everyone soon. Also, if anyone else is going through this and wants to exchange email addresses so we can share any useful information we find out with each other, please let me know.
Best, Joe
Hi, Joe!
I developed this exact same issue a month ago. My sleep doctor confirmed that it's called sleep-onset central sleep apnea. From what I understand, the causes could be idiopathic or could be from something serious like heart failure. It's best to get tested in case you already haven't.
As for treatment, I was told that Acetazolamide is actually used off label to treat central sleep apnea. I hope that you've found a solution to your problem already, but if you haven't, I would definitely recommend considering this medication. I haven't tried it yet as it was just brought to my attention, but I just might if I don't find any other good solutions.
Hope you're doing well!
I have been experiencing the exact same thing over the past year. Just as I am falling asleep, I snort and gasp for air. I was originally diagnosed with mild to moderate OSA. I tried the cpap machine but just couldn’t sleep with the irritation. It just seemed like my sleep doctor was pushing the machines and not really trying to figure out what was wrong. 6 weeks ago I had surgery to remove my tonsils, shorten my palette, straighten out my deviated septum and reduce my tongue. This was an extremely painful recovery. Unfortunately I still wake myself up every night just as I am falling asleep snoring or gasping for air. In the morning I wake up and try to fall back asleep but it continues to wake me. One other weird thing is that I also have random muscle spasms and muscle jerks right as I fall asleep. My arm will suddenly move or my whole chest will lurch forward. This is so fripustrating. It just seems like there is no light at the end of the tunnel.
I think a CPAP would have to be set up a bit differently to address the issue of apnea just as you are going to sleep. Typically the pressure is either held low or ramped up slowly to make it more comfortable to go to sleep. However, to stop an apnea that happens right when you are going to sleep would require higher pressure earlier. I think one would want not use a pressure ramp at all and start at the full treatment pressure, or use a very short 5 minute ramp so it would be at full treatment pressure BEFORE you go to sleep. And the other issue is that a CPAP cannot prevent a clear airway or central apnea event at all. Pressure does not help when the airway is already open. The CPAP would only help if the sleep onset apnea was of the obstructive type.
I had the same issue for several months this summer. I kept trying to doze off to sleep, then would wake up. I eventually bought a Contec SpO2 watch with O2 finger sensor. I wear it at night to record what was going on. Immediately upon falling asleep, I'd have transitional Central Apneas happen. Then I'd wake up immediately upon dozing. It would repeat and repeat. I'd eventually give up trying to get to sleep and wouldn't sleep for a night.
I also had crazy random muscle spasms and jerks, especially in my neck and head area. My doctors claimed it was all "stress" and "anxiety" causing these symptoms. They had no solution, and I even went to the ER twice this year because I couldn't get to sleep.
I did find out though, that in May I had DVT/PE (blood clots in lungs), and I was in the hospital for a few days. During a couple nights, I told them to monitor my O2 levels which they did. The hospital O2 alarm kept going off, because my O2 would drop, just like it did when I was at home. And I would have the same terrible Central Apneas happen. This continued to happen for a week or longer after I was home and put on blood thinners. But it has since gone away for the most part.
I also found out I had gallstones, and during the day I had this "unwell" feeling all the time. Especially after eating and taking my Multaq and Bystolic for AFIB. I thought it could be medicine causing the issue. But I think all of these symptoms were caused due to a combination of my anxiety/panic disorder, blood clots, and the gallstones.
So far for the last couple of months, I haven't experienced any transitional Central Apneas. But I do occasionally wake up and have insomnia. I take a very low dose of Klonopin and Melatonin at night to sometimes sleep. This helps, and doesnt seem to affect my breathing.
My only current issue is that I still get dizziness and feel faint when I stand up sometimes! Last night I was on my couch, I stood up, and immediately the room started spinning, and I felt like I was going to pass out. I took my Blood Pressure and it was a little high, 153/90. Went to the clinic this morning and they had no answers. An EKG was normal.
Are you taking any kind of blood pressure medication? What you describe is called orthostatic hypotension. It can be a side effect of a blood pressure med, and of course other things. You have to check blood pressure immediately on standing to detect it.
Hi, That is exactly what happens to me. I have had this thing for 7 years now. I already know some things that trigger it like eating too late at night, eating too much, drinking/eating: chocolate, coffee, wine, beer, tomato sauce, sodas, all of them in the afternoon. I also get it if I am anxious, stressed or being under an allergic attack. ( reflux has been already clinically ruled out) I also know that if I exercise hard at night I got less chances of having an apnea attack. If I drink two drinks of vodka I might not get it. I know that if I try to be physically tired or relaxed with alcohol I might get into the deep part of sleep at once, skipping the two first hours of light sleep which is the part when the attacks are triggered. I have never used benzodiazepines and I won’t do it because I have seen the consequences in others. I will be under a new treatment soon. I will let you guys know. Cheers
Hey Folks, Stumbled on this site/post while desperately searching for answers as I have this same issue. Have been on CPAP for almost 5 years now. Had some trouble adjusting to it for the first 3 months but since then, no issues.
I do experience sleep issues relative to anxiety every 3-5 years. I'm actually dealing with this now.
The primary experience I have is the same mentioned hear. It causes me to become very anxious and I've developed a fear of going to bed.
I'm 95% certain the problem is associated to anxiety. I think these events probably occur normally but I don't notice them because I'm in a more relaxed state of mind and continuing to fall asleep.
During times of high anxiety, I'm aware of all bodily sensations that normally wouldn't get a second thought.
My sleep doctor suggested changing the EPR setting on my Resmed S9 Elite. It was set to 3 and I lowered it to 2. That night, I had no issues.
However, because my anxiety is still high and I'm going through an online CBT-I program (and I just broke my ankle so sleeping with a boot on) my CA's during sleep initiation are a problem again.
I don;t know this for certain but after all the research I've done, the answer is likely to be lowering my base level anxiety.
Only a 7 day user of BPAP Resmed Aircurve 10 S, so no inputs on those. Still trying to get a mask to work well. For those who mentioned anxiety and energy level suspicions, you might look into acupuncture and/or using CBD hemp oil. The oil seems to have helped my edginess and anxiety in last 30 days. When asking Drs. about CBD they smile and offer no opinions. Many users claim it helps them. Some of my Drs.have patients who claimed it helped. It's pretty new and big Pharma can't make any money on it. We're on our own out here. I thank contributors on this Forum and God, hoping we all get better.
I have been using hemp CBD oil for two weeks and it is working wonderful for me, it is even lowering my AHIs... I also fall sleep Inmediately, so no more insomnia and panic/anxiety...today I am testing my urine for marijuana traces just to confirm that my treatment does not have THC susbtance in it.
Hello Charming Coyote and fellow transitional apnea sufferers,
This thread is over 3 years old but I'm going to take a shot in the dark and post here in the hopes that someone will read this.
I have begun suffering from the same issue. Just as I fall asleep and transition into a dream state my breathing either ceases or becomes extremely shallow. I immediately pop awake, probably as an instinctual fear response to the threat of suffocation. Either the condition or my fear of it keeps me awake all night long despite changing my sleeping position, changing beds, or attempts at relaxing myself. It's maddening. Thankfully, this doesn't occur every night but I worry that it will eventually.
I have not yet seen a doctor or undergone a sleep study but I have scheduled it. My wife tells me that i am restless at night and frequently wake up gasping (although i have no memory of these episodes), so I believe I suffer from general CSA. I am otherwise healthy as far as I know, with the exception of frequent acid reflux, for whatever that's worth.
Has anyone in this thread suffering from this found relief since it was posted? Has anyone determined the cause? If so, please share what solution(s) finally worked for you. I suspect stress plays a role in this but it cant be the only reason as I'm not particularly stressed these days and the vast majority of people endure stress without feeling like they will die in their sleep.
Thanks in advance for any help or advice. -Marc
There are two basic types of apnea events where the airflow stops. One is obstructive where the airway is blocked, and is called obstructive apnea. The other is when you simply do not breathe. It is called central or clear airway apnea. If you get a CPAP machine they will be quite effective at reducing or eliminating obstructive events. If the event you are getting just as you go to sleep is obstructive in nature, then you will want to have the machine set so air pressure is up to normal or at least higher while you are going to sleep. If it is caused by you simply stopping to breathe then it is more difficult to prevent. And if that is the only type of event you have then a CPAP machine may not be a solution. One nice thing about a CPAP is that you can download software that lets you view your air flow minute to minute as you sleep. This software would let you determine in much more detail when these events occur. They may be able to do this in a sleep study as well, but it is time consuming to look at every breath you take even over a spread of 30 minutes or so, and they may not do that as a matter of routine.
Hope that helps some,
Hello CharmingDesertSandCoyote0755
First of all, I am also in a similar situation. A lot of transitional/sleep onset apneas .. I tried ramps, setting EPR on my Air sense , but nothing helped. What seemed to help me was some breathing exercises like Vim hof breathing (see link below). I still get them, but at a reduced rate..
But you said you are an asthma patient, so I wouldn't reccomned them to you without checking with you doctor first ..
Any updates? I am suffering from the same thing. Just made a separate thread about it.
My sleep doctor claims it's all in my head and that it's all anxiety related. Well, my general doctor gave me meds for anxiety. They seem to be helping with the anxiety, but not the sleep onset apneas. Now I lie in bed feeling calm as I still get joleted awake every time I drift off to sleep. It's nice to feel calm, but it would be nicer to actually be able to sleep!
i am dealing with the same!! please help. have been 2 constantly years. every single day
i have anxiety , i have sleep apnea but i have CPAP- i went to 6 differenten sleep specialists, no one cure me of this awakeing just as falling asleep. several meds and nothing...
Please give me smoething guys..
Thank youu
I dont know how old this is but I'm suffering from the same thing it seems. I am jerking awake every time I fall asleep and my mental health is so bad. After reading this I am absolutely terrified that nothing will ever help. Has anyone gotten anywhere? I assumed I had OSA because I am overweight and I snore, but maybe its not that. I haven't had the results of my sleep study yet but have been using a cpap I bought, but I still jerk awake. I feel like I am going insane. I can't live like this much longer
Hello! I have good news for you. After going through many tests, it was discovered that my autonomic nervous system was acting up. My sympathetic nervous system was working a bit too well, which caused my body to get that adrenaline rush that jerked me awake everytime I tried to fall asleep.
Two things solved this problem. First, I got put on a Beta Blocker called Nadolol. It’s only 10mg once per night and I have no side effects. I swear it saved my life because I too was losing my mind over not being able to sleep. I was also terrified to even try sleeping.
Second thing is not getting yourself overly tired. The more tired you are, the more likely it is that those jerks will happen.
Please see about a Beta Blocker! Your autonomic nervous system might just be a little too active. It happens.
Let us know!
Hi - finally someone giving some way out… thanks @amberfalcon -
Is it safe to take that nadonol? Did your doctor say yes to it? No side effects or something like that? Just scared but will try thanks
Indeed! Nadolol is one of the safest beta blockers out there with the least amount of side effects. I’ve been through the gambit of beta blockers and hated Propranolol and Metoprolol. They caused so many issues, especially further issues with sleep. But Nadolol is one of the best meds I’ve ever taken.
I actually had to go to Mayo for all of my health issues. The neurologist I saw put me on Nadolol for the autonomic nervous system issues.
I think for those of us that aren’t finding relief in CPAPs or standard apnea treatments are probably dealing with a heightened sympathetic nervous system, which is what causes that anxious feeling. It’s not always psychological. Sometimes it truly is the body, in this case the autonomic nervous system, that was the issue.
I would definitely talk to one of your doctors about it, make sure it doesn’t interact with any meds you might be taking, and start at a low dose.
Hi First of all thank you so much for taking the time to reply I really appreciate it! I've been seeing things similar to this and I must admit I've wondered if it has to do with my anxiety, which is always high but obviously in over drive when I can't sleep. That seems to be the catch 22 here because how can I control my anxiety if I can't sleep? I have a genuine fear of not sleeping now as I've suffered from long bouts of insomnia as well. It just seems to never end! I did consider beta blockers but I've heard they sometimes make it hard to sleep too so I was afraid to try. I suppose it's worth a shot though. I think you're onto something with your nervous system sending a rush of adrenaline I've definitely felt that. It's just confusing to me because other times I wake up and clearly haven't been breathing so is it sleep apnea or not? Thanks again sorry for the long reply
No worries!
Some beta blockers due indeed make sleep more difficult. Some have even made breathing more difficult for me. The two biggest culprits of that were Propranolol and Metoprolol.
When my neurologist wanted to be me on Nadolol for autonomic nervous system issues I was SO nervous, but he was very reassuring. And sure enough, it helped so many things. What I thought was anxiety wasn’t. It’s amazing how the body can impact the mind.
I wonder if you know why nadonol worked and the other two did not? I've asked for beta blockers before and was put on propranolol for anxiety and it didn't seem to help. I'm not sure if I can get nadonol where I am (scotland) but it would help if I knew what it was about this one in connection to the central nervous system? I obviously do struggle with anxiety as well but you're saying it's not that? Isn't this central nervous system issue kind of set off because of anxiety? Sorry I'm just a bit confused Thanks again!
The autonomic nervous system is part of the nervous system, and your sympathetic/parasympathetic nervous system are parts of your autonomic nervous system.
Sometimes the sympathetic nervous system gets stuck in the “on” position and overrides the parasympathetic nervous system. The sympathetic nervous system is the fight/flight bit, whereas the parasympathetic nervous system is the calming bit.
When the sympathetic nervous system is stuck in the “on” position, it feels like you have an anxiety or panic disorder. Keep in mind, many people do experience anxiety and panic because of chemical imbalances in their brains, but many of us also feel anxiety and panic not because of a chemical imbalance in our brains, but because of an autonomic nervous system that isn’t working properly.
I had been to many therapists and psychiatrists, had been told it was anxiety and panic disorder, was put on so many different meds, etc. None of them worked. When I went on Nadolol (also known as Corgard), my sympathetic nervous system calmed down, which basically means it wasn’t constantly sending the “Panic!” signal to my brain.
You may very well have anxiety. I definitely can’t tell you one way or another. I can only speak to my experience and what my neurologist has told me other patients of theirs have experienced.
I’m also not sure why Nadolol worked so much better, but that is his preferred beta blocker to use, which is interesting because Cardiologists prescribe Propranolol and Metoprolol like it’s candy.
Ok that makes sense. I've definitely had anxiety seemingly for no reason all my life So I wonder if that's maybe what's causing my nervous system to be in overdrive, or the other way around? Maybe it doesn't matter. I'm definitely going to work on my anxiety and breathing but hopefully a beta blocker could help take the edge off too. It seems to just be a cycle that feeds itself. My last question to you is how do I find out if my nervous system is in overdrive? Is there a way to diagnose this? Would I need to be referred to a neurologist? I do worry that I might be put on a different beta blocker but I did read that they are prescribed for high blood pressure, which I've just found out I have and I also read that can be a symptom of over active nervous system ( I know I'm not wording that right but you know what I mean haha) So that all seems to make sense to me! Thank you again so much for all your help I feel like I'm finally on the road to sorting this out. You could be a genuine life saver!
It’s a chicken or the egg situation, for sure. Sometimes we can’t know 100% which came first, but it’s totally possible that it’s your autonomic nervous system.
There are tests that cardiologists and/or neurologists can do to see if your autonomic nervous system is acting up. Here are some:
-Tilt Table Test -Valsalva Maneuver Test Deep Breathing Test -Quantitative Sudomotor Axon Reflex Test (QSART) -Thermoregulatory Sweat Test (TST)
Here’s more info! https://medlineplus.gov/lab-tests/autonomic-testing/
This is all so helpful! I've done a lot of research today and I really think you are right. I have a lot of the other symptoms of an over active nervous system too. I can't thank you enough for all your help. It seems the people on here are way more clued up that any doctor I've spoken to. Thanks again!
Amber, Thanks for sharing. I've been diagnosed with a form of Dysautonomia a year and 1/2 ago. The transitional sleep apnea began about 1 year ago after a major surgery--at least that's when I first realized it was happening. I've had other sleep apnea issues for years. My sleep doctor also believes I may have narcolepsy as I go directly to REM sleep. I hadn't heard about beta blockers as treatment until your post. For me, anything that slows down my central nervous system exacerbates the TSA so I'm not sure if it would benefit me. Though, I actually have found two things that lower my incidence of transitional sleep apnea-B12 injections and PEMF therapy as well as when I do all my therapies that my functional neurologist prescribed. They are out of the box in their treatments but specialize in Dysautonomia and helped me get and stay stable. I have flares of the TSA just like I have flares of Dysautonomia, but they don't necessarily coincide. I take 6 mg of timed release melatonin, 200 mg L-theanine and Calm magnesium each night to get to sleep. I also find that I do better if I do a lot of physical exertion because I fall asleep quicker. We're all different and my sleep doctor said my issues are vey complicated and he suspects an autoimmune component. Anyway, I just thought I'd comment in case something in my experience is helpful to someone. I haven't conquered this yet as I'm still working through getting the right PAP therapy. I have failed so far on an APAP, but the sleep doctor wanted to try one more setting--and in the week since, I've been worse. I've qualified for a BIPAP at my last sleep study, so that's next. In the meantime, I'm going to try to be more disciplined in doing all the things that have helped.
Interesting that you found some relief from a beta blocker. My biggest issue with using a CPAP has been central apnea events. Rightly or wrongly I decided that the beta blocker I was taking for blood pressure control may have been a contributing factor. It slows your heart rate down, and my theory was that it reduced blood circulation rate and upset the breathing control system. It depends on detecting the CO2 level in your blood and provides the feedback that your are breathing too fast or too slow. In any case I told my doctor about my theory, and while I think he was skeptical (he is a GP, not a sleep specialist), he agreed to cutting the dose I was taking. I was on 5 mg of Bisoprolol in the mornings. This was reduced to 2.5 mg (by splitting the 5 mg pills) taken in the mornings. I can't be 100% sure this is the reason, but I now average less than 1.0 for an AHI. CA events are still the majority of my events, but they are way lower than I was getting before.
In any case a beta blocker may help relax you, but the amount you want to relax may vary from person to person. I would just watch that CA event frequency does not become an issue. Central apnea is very individual specific.
Hello, I still occasionally suffer from this, but I have gathered some insights that may or may not be helpful.
I am more likely to experience transitional apnea if I have been staring at a screen for an extended time in the evening. Try limiting your screen time.
I find that I naturally want to fall asleep at 11pm or so. Those nights where I stay up much later for whatever reason are nights that I have difficulty falling asleep and I will also often wake up gasping when I finally manage to do so. If I simply let myself fall asleep on the couch watching TV I seem to have no apnea episodes. So following your body's preferred sleep schedule might be helpful.
Finally. I read somewhere that practicing holding your breath for as long as you can can be useful. The sudden waking we suffer is a result of our body's CO2 sensor being too easily triggered by the slightly elevated CO2 in our blood following that short period of paused breathing that normally occurs as we transition into sleep. By training yourself with breath holding you are decreasing your body's sensitivity to carbon dioxide and giving your brain the time it needs to fall asleep and return to automatic breathing. I haven't put this into practice yet but I thought it made sense.
If anyone has their own tips I'd love to hear them.
Good luck out there friends.
I have been dealing with those symptoms as well. So scary. I went to the emergency room for being 5 nights with almost no sleep. I was prescribed trazodone which worked for three or four nights, but everything came back, for two nights I hardly slept at all. I feel a lot of anxiety, my heart races, my whole body shakes... I'm really panicked. full of sleep and I can't sleep because I barely fall asleep "something" wakes me up.... What pills do you take to Help relax to sleep?
I'm sure I have made this comment before, but the first thing I would do if I was having suspected transitional sleep apnea events would be to document that I am actually having an apnea event while going to sleep. With OSCAR it should be fairly easy to do that. I don't know how one could treat this condition until one confirms that apnea events are actually occurring, and what type they are; central or obstructive.